Abstract
Persistensi penggunaan obat antihipertensi pada pasien hipertensi sangat diperlukan mengingat hasil utama terapi hipertensi adalah mencegah kejadian penyakit kardiovaskular seperti infark miokard, dan stroke yang berujung pada kematian. Penelitian ini bertujuan mengetahui pengaruh jenis terapi dan jenis obat antihipertensi terhadap persistensi. Penelitian ini menggunakan desain studi kohort retrospektif dan menggunakan sumber data sekunder pasien hipertensi rawat jalan peserta asuransi kesehatan PT Askes di RSUD Panembahan Senopati Bantul. Metode pengukuran persistensi adalah metode the gaps between refill dengan tenggang waktu pengambilan obat selama 30 hari. Data dianalisis menggunakan uji kai kuadrat, Kaplan-Meier, dan Cox regression. Jumlah subjek yang ikut dalam penelitian ini adalah 304 pasien hipertensi yang menggunakan obat antihipertensi pertama kali (tanggal indeks diagnosis 1 Juli 2007 hingga 31 Desember 2008). Setelah pengamatan 4,5 tahun, hampir separuh subjek yang mendapat monoterapi (57,6%) dan kombinasi terapi (53,8%) tidak persisten menggunakan obat antihipertensi. Ketidakpersistenan penggunaan obat antihipertensi lebih besar pada kelompok monoterapi daripada kelompok kombinasi, tetapi perbedaan tersebut tidak signifikan (RR = 0,94; 95% CI = 0,73 - 1,21). Penggunakan diuretik (85,7%) dan kombinasi obat diuretik + ACE inhibitor (84,6%) cenderung tidak persisten dibandingkan subjek yang menggunakan ACE inhibitor (58,4%). Perbedaan ini bermakna secara statistik (RR = 1,47; 95% CI = 1,05 - 2,01 dan RR = 1,45; 95% CI = 1,10 - 1,91). Persistensi dipengaruhi oleh jenis obat antihipertensi yang digunakan, yaitu ACE inhibitor. Persistence of the use of antihypertensive drugs in hypertensive patients greatly needed. Considering the primary outcome of treatment for hypertension is to reduce or prevent the occurrence of cardiovascular events such as myocardial infarction, stroke resulting in the risk of death. This study aims to determine whether persistence is influenced by the type of treatment or type of antihypertensive drugs. This study was designed with retrospective cohort study using database of prescribing claimed of subjects under health insurance (PT Askes) in Panembahan Senopati hospitals using antihypertensive drugs. Persistency measurement method used is the method of the gaps between refilling. The grace period taking the drug for 30 days. Further data were analyzed using the chi square test, Kaplan-Meier, and Cox regression. This cohort study involving 304 patients using antihypertensive medications first (index diagnosis 1 July 2007 until 31 December 2008). After observation for 4,5 years found almost half of the subjects receive monotherapy (57,6%) or combination therapy (53,8%) are not persistent in the use of antihypertensive medications. Not persistent greater in the monotherapy compare to combination therapy group. However, this difference did not reach significance (RR = 0,94; CI 95% = 0,73 - 1,21). Subject were using a diuretic (85,7%) and ACE inhibitor + diuretic combination (84,6%) tends not to be persistent compare to subject using ACE inhibitors (58,4%). This difference was statistically significant (RR = 1,47; CI 95% = 1,05 - 2,01 and RR = 1,45; CI 95% = 1,10 - 1,91). Overall, persistence is influenced by the type antihypertensive drugs used, the ACE inhibitors.
References
1. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005; 365: 217-23. 2. Departemen Kesehatan Republik Indonesia. Laporan hasil riset kesehatan dasar (Riskesdas) nasional 2007. Jakarta: Badan penelitian dan pengembangan kesehatan, Departemen kesehatan Republik Indonesia; 2008. 3. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003; 43: 1206-52. 4. Prandin MG, Cicero AFG, Veronesi M, Cosentino E, Dormi A, Strocchi E, et al. Persistence on treatment and blood pressure control with different first-line antihypertensive treatments: a prospective evaluation. Clinical and Experimental Hypertension. 2007; 29: 553-62. 5. Fox KM. EURopean trial on reduction of cardiac events with perindopril in stable coronary artery disease Investigators, efficacy of perindopril in reduction of cardiovascular events among patient with stable coronary artery disease: randomised, double-blind, placebo-controlled, multicentre trial (The EUROPA Study). Lancet. 2003; 362(9386): 782-8. 6. Mazzaglia G, Ambrosioni E, Alacque M, Filippi A, Sessa E, Immordino V, et al. Adherence to antihypertensive medication and cardiovascular morbidity among newly diagnosed hypertensive patient. Circulation. 2009; 120: 1598-605. 7. Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Medical Care. 2005; 43(6): 521-30. 8. Bertrand ME, Remme WJ, Fox KM, Simoons ML, and EUROPA investigators. Effects of perindopril on long term clinical outcome of patients with coronary artery disease and preserved left ventricular function. International Journal of Cardiology. 2007; 121(1): 57-61. 9. Sikka R, Xia F, Aubert RE. Estimating medication persistency using administrative claims data. American Journal of Managed Care. 2009; 11(7): 449-57. 10. Lachaine J, Petrella RJ, Merikle E, Ali F. Choices, persistence and adherence to antihypertensive agents: evidence from RAMQ data. Canadian Journal of Cardiology. 2008; 24(4): 269-73. 11. Hasford J, Bernhardi DS, Rottenkolber M, Kostev K, Dietlein G. Persistence with antihypertensive treatments: result of a 3-year followup cohort study. European Journal of Clinical Pharmacology. 2007; 63: 1055-61. 12. Allhat. What has it taught us so far? Canadian Medical Association Journal. 2004; 171: 719-20. 13. Polluzi E, Strahinja P, Vargiu A, Chiabrando G, Silvani MC, Motola D, et al. Initial treatment of hypertension and adherence to therapy in general practice in Italy. European Journal of Clinical Pharmacology. 2005; 61: 603-9. 14. The ALLHAT Collaborative Research Group. Blood pressure control by drug group in the antihypertensive and lipid-lowering treatment to prevent peart attack trial (ALLHAT). Journal of Clinical Hypertension. 2008; 10: 751-60. 15. Matchar DB, McCrory DC, Orlando LA, Patel MR, Patel UD, Patwardhan MB, et al. Systematic review: comparative effectiveness of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers for treating essential hypertension. Annals of Internal Medicine. 2008; 148: 16-29. 16. Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients, the hearth outcomes prevention evaluation study investigators. New England Journal of Med0icine. 2000; 342(2): 145-53. 17. Donnely R, Manning G. The PEACE trial investigators, angiotensinconverting-enzyme inhibition in stable coronary artery disease. New England Journal of Medicine. 2004; 351(20): 2058-68. 18. Zidek W, Schrader J, Luders S, Matthaei S, Hasslacher C, Hoyer J, et al. Ramipril-based versus diuretic-based antihypertensive primary treatment in patient with pre-diabetes (AdaPT) study. Cardiovascular Diabetology. 2012; 11: 1-11. 19. Pilot L, Abrahamowicz M, Eisenberg M, Humphries K, Behlouli H, Tu JV. Effect of different angiotensin-coverting-enzyme inhibitors on mortality among elderly patient with congestive heart failure. Canadian Medical Association Journal. 2008; 178(10): 1303-11. 20. Mann JF, Gerstein HC, Yi QL, Lonn EM, Hoogwerf BJ, Rashkow A, et al. Development of renal disease in people at high cardiovascular risk: result of the HOPE randomized study. Journal of the American Society of Nephrology. 2003; 14(3): 641-7. 21. Billic M, Munjas-Samarin R, Ljubanovic D, Horvatic I, Galesic K. Effect of ramipril and valsartan on proteinuria and renal function in patient with nondiabetic proteinuria. Collegium Antropologicum. 2011; 35(4): 1061-6. 22. Sheppard RJ, Schiffrin EL. Inhibition of the renin-angiotensin system for lowering coronary artery disease risk. Current Opinion in Pharma cology. 2013; 13: 274-9. 23. Zygmuntowicz M, Owczarek A, Elibol A, Olszanecka-Glinianowicz M, Chudek J. Blood pressure for optimal health-related quality of life in hypertensive patients. Journal of Hypertension. 2013; 31(4): 830-9. 24. ONTARGET Investigator. The cost implication of the use of telmisartan or ramipril in patients at high risk for vascular events: the ONTARGET study. Journal of Medical Economics. 2011; 14(6): 792-7. 25. Borghi C, Ambrosioni E, Ombini S, Cicero AFG, Bacchelli S, Esposti DD, et al. Cost-effectiveness of zofenopril in patient with left ventricular systolic disfunction after acute myocardial anfarction: a post hoc analysis of SMILE-4. Clinico Economic and Outcomes Research. 2013; 5: 317-25.
Recommended Citation
Nurmainah N , Ahmad A , Dwiprahasto I ,
et al.
Persistensi Penggunaan Obat Antihipertensi pada Pasien Hipertensi Rawat Jalan.
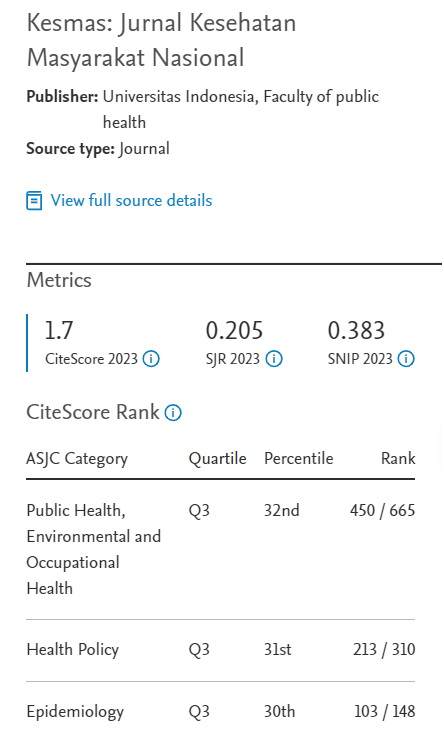
Kesmas.
2013;
8(1):
13-18
DOI: 10.21109/kesmas.v8i1.336
Available at:
https://scholarhub.ui.ac.id/kesmas/vol8/iss1/3