Abstract
Telemedicine’s adoption has been effective in certain contexts despite being controversial in certain settings because of its tendency to cause misdiagnosis and concerns about data privacy. This study aimed to synthesize the research findings on the factors leading to the adoption of telemedicine among developing economies. The study utilized Preferred Reporting Items for Systematic Reviews and Meta-Analysis methodology to analyze 27 related literature and the Unified Theory of Acceptance and Use of Technology to map out the factors considered enablers and barriers in adopting telemedicine. Results showed that performance expectancy, effort expectancy, social influence, and facilitating conditions were significant predictors. However, the study also underscored that the lack of information and communications technology support, lack of resources, lack of organizational effectiveness, lack of quality care, lack of motivation, lack of trustworthiness, and lack of user satisfaction were predominant hindrances at both individual and organizational levels. This analysis on the enablers and barriers of telemedicine adoption hopes to contribute strategic recommendations that practitioners in public health, decision-makers in global health policy, technology developers, and future research may explore to expand the existing knowledge on the optimal adoption of telemedicine in developing economies.
References
1. Tripepi M, Pizzocaro E, Giardino A, et al. Telemedicine and pancreatic cancer: A systematic review. Telemed J E Health. 2022; 29 (3): 352–360. DOI: 10.1089/tmj.2022.0140.
2. Hopkins BS, Cloney MB, Texakalidis P, et al. Outpatient telemedicine in neurosurgery: 15,677 consecutive encounters in a comparative analysis of its effectiveness and impact on the surgical conversion rate. J Neurosurg. 2023; 139 (5): 1446–1455. DOI: 10.3171/2023.2.JNS221477.
3. Alsabeeha NHM, Atieh MA, Balakrishnan MS. Older adults’ satisfaction with telemedicine during the COVID-19 pandemic: A systematic review. Telemed J E Health. 2022; 29 (1): 38–49. DOI: 10.1089/tmj.2022.0045.
4. Elawady A, Khalil A, Assaf O, et al. Telemedicine during COVID-19: A survey of health care professionals’ perceptions. Monaldi Arch Chest Dis. 2020; 90: 1528. DOI: 10.4081/monaldi.2020.1528.
5. Shaikh A, Khan M, Ismail FW. Experience of telemedicine in gastroenterology outpatient practice during the COVID-19 pandemic: Experiences from a tertiary-care hospital in a developing country. Clin Exp Gastroenterol. 2022; 15: 91–99. DOI: 10.2147/CEG.S361381.
6. Zobair KM, Sanzogni L, Sandhu K. Telemedicine healthcare service adoption barriers in rural Bangladesh. Australas J Inf Syst. 2020; 24: 1–24. DOI: 10.3127/ajis.v24i0.2165.
7. Hoque MR, Bao Y, Sorwar G. Investigating factors influencing the adoption of e-health in developing countries: A patient’s perspective. Inform Health Soc Care. 2016; 42 (1): 1–17. DOI: 10.3109/17538157.2015.1075541.
8. Alajlani M, Clarke M. Effect of culture on acceptance of telemedicine in Middle Eastern Countries: Case study of Jordan and Syria. Telemed J E Health. 2013; 19 (4): 305-311. DOI: 10.1089/tmj.2012.0106.
9. Chandwani RK, Dwivedi YK. Telemedicine in India: Current state, challenges and opportunities. Transform Gov People Process Policy. 2015; 9 (4): 393–400. DOI: 10.1108/TG-07-2015-0029.
10. Kruse CS, Williams K, Bohls J, et al. Telemedicine and health policy: A systematic review. Health Policy Technol. 2021; 10 (1): 209–229. DOI: 10.1016/j.hlpt.2020.10.006.
11. Bokolo A. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020; 44: 132. DOI: 10.1007/s10916-020-01596-5.
12. Sagaro GG, Battineni G, Amenta F. Barriers to sustainable telemedicine implementation in Ethiopia: A systematic review. Telemed Rep. 2020; 1 (1): 8–15. DOI: 10.1089/tmr.2020.0002.
13. Abdullrahim A, De Coster R. A framework of e-health systems adoption and telemedicine readiness in developing countries. 2016 Int Conf Inf Society (i-Society). 2016; 1: 105–108. DOI: 10.1109/i-Society.2016.7854188.
14. Adenuga KI, Iahad NA, Miskon S. An initial model for telemedicine adoption in developing countries. ARPN J Eng Appl Sci. 2015; 10 (23): 17614– 17623.
15. Kruse CS, Karem P, Shifflett K, et al. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare. 2018; 24 (1): 4–12. DOI: 10.1177/1357633X16674087.
16. Adenuga KI, Iahad NA, Miskon S. Towards reinforcing telemedicine adoption amongst clinicians in Nigeria. Int J Med Inf. 2017; 104: 84-96. DOI: 10.1016/j.ijmedinf.2017.05.008.
17. Rahi S, Khan MM, Alghizzawi M. Factors influencing the adoption of telemedicine health services during COVID-19 pandemic crisis: An integrative research model. Enterp Inf Syst. 2021; 15 (6): 769–793. DOI: 10.1080/17517575.2020.1850872.
18. Yamin MAY, Alyoubi BA. Adoption of telemedicine applications among Saudi citizens during COVID-19 pandemic: An alternative health delivery system. J Infect Public Health. 2020; 13 (12): 1845–1855. DOI: 10.1016/j.jiph.2020.10.017.
19. Luciano E, Mahmood MA, Mansouri Rad P. Telemedicine adoption issues in the United States and Brazil: Perception of health professionals. Health Informatics J. 2020; 26 (4): 2344–2361. DOI: 10.1177/1460458220902957.
20. Ghani MKA, Jaber MM. The effect of patient privacy on telemedicine implementation in developing countries: Iraq case study. Res J Appl Sci Eng Technol. 2015; 11 (11): 1233–1237. DOI: 10.19026/rjaset.11.2230.
21. Alboraie M, Allam MA, Youssef N, et al. Knowledge, applicability, and barriers of telemedicine in Egypt: A national survey. Int J Telemed Appl. 2021; 5565652. DOI: 10.1155/2021/5565652.
22. Al-Samarraie H, Ghazal S, Alzahrani AI, et al. Telemedicine in Middle Eastern countries: Progress, barriers, and policy recommendations. Int J Med Inf. 2020; 141: 104232. DOI: 10.1016/j.ijmedinf.2020.104232.
23. Chao CM. Factors determining the behavioral intention to use mobile learning: An application and extension of the UTAUT model. Front Psychol. 2019; 10: 1652. DOI: 10.3389/fpsyg.2019.01652.
24. Aranha M, Shemie J, James K, et al. Behavioural intention of mobile health adoption: A study of older adults presenting to the emergency department. Smart Health. 2024; 31: 100435. DOI: 10.1016/j.smhl.2023.100435.
25. Alam MZ, Hoque MR, Hu W, et al. Factors influencing the adoption of mHealth services in a developing country: A patient-centric study. Int J Inf Manag. 2020; 50: 128–143. DOI: 10.1016/j.ijinfomgt.2019.04.016.
26. Zobair KM, Sanzogni L, Sandhu K. Expectations of telemedicine health service adoption in rural Bangladesh. Soc Sci Med. 2019; 238: 112485. DOI: 10.1016/j.socscimed.2019.112485.
27. Kamal SA, Hussain S, Shafiq M, et al. Investigating the adoption of telemedicine services: An empirical study of factors influencing physicians’ perspective in Pakistan. The Nucleus. 2018; 55 (3): 153–163.
28. Kamal SA, Shafiq M, Kakria P. Investigating acceptance of telemedicine services through an extended technology acceptance model (TAM). Technol Soc. 2020; 60: 101212. DOI: 10.1016/j.techsoc.2019.101212.
29. Xue Y, Liang H, Mbarika V, et al. Investigating the resistance to telemedicine in Ethiopia. Int J Med Inf. 2015; 84 (8): 537–547. DOI: 10.1016/j.ijmedinf.2015.04.005.
30. Jayasinghe D, Crowder RM, Wills G. Model for the adoption of telemedicine in Sri Lanka. SAGE Open. 2016; 6 (3): 1–10. DOI: 10.1177/2158244016668565.
31. Adenuga KI, Iahad NA, Miskon S. Telemedicine system: service adoption and implementation issues in Nigeria. Indian J Sci Technol. 2020; 13 (12): 1321–1327. DOI: 10.17485/IJST/v13i12.180.
32. Ramírez-Rivas C, Alfaro-Pérez J, Ramírez-Correa P, et al. Predicting telemedicine adoption: An empirical study on the moderating effect of plasticity in Brazilian patients. J Inf Sys Eng Manag. 2021; 6 (1): em0135. DOI: 10.29333/jisem/9618.
33. Latifi F, Alizadeh S. The influence of national factors on transferring and adopting telemedicine technology: Perspectives of chief information officers. Int J E Health Med Commun. 2016; 7 (3): 52–65. DOI: 10.4018/ijehmc.2016070104.
34. Chowdhury SR, Sunna TC, Ahmed S. Telemedicine is an important aspect of healthcare services amid COVID-19 outbreak: Its barriers in Bangladesh and strategies to overcome. Int J Health Plann Manage. 2021; 36 (1): 4–12. DOI: 10.1002/hpm.3064.
35. Cilliers L, Flowerday S. User acceptance of telemedicine by health care workers: A case of the Eastern Cape Province, South Africa. Electron J Inf Syst Dev Ctries. 2014; 65 (1): 1–10. DOI: 10.1002/j.1681-4835.2014.tb00467.x.
36. Dodoo JE, Al-Samarraie H, Alzahrani AI. Telemedicine use in Sub-Saharan Africa: Barriers and policy recommendations for COVID-19 and beyond. Int J Med Inf. 2021; 151: 104467. DOI: 10.1016/j.ijmedinf.2021.104467.
37. Hosseini SM, Boushehri SA, Alimohammadzadeh K. Challenges and solutions for implementing telemedicine in Iran from health policymakers’ perspective. BMC Health Serv Res. 2024; 24: 50. DOI: 10.1186/s12913-023-10488-6.
38. Bakshi S, Tandon U. Understanding barriers of telemedicine adoption: A study in North India. Syst Res Behav Sci. 2022; 39 (1): 128–42. DOI: 10.1002/sres.2774.
39. Schmitz A, Díaz-Martín AM, Yagüe Guillén MJ. Modifying UTAUT2 for a cross-country comparison of telemedicine adoption. Comput Hum Behav. 2022; 130: 107183. DOI: 10.1016/j.chb.2022.107183.
40. Wu TC, Ho CTB. Barriers to telemedicine adoption during the COVID-19 pandemic in Taiwan: Comparison of perceived risks by socioeconomic status correlates. Int J Environ Res Public Health. 2023; 20 (4): 3504. DOI: 10.3390/ijerph20043504.
Recommended Citation
Macabato Z , Velasco L , Escabarte A ,
et al.
Telemedicine Adoption in Developing Economies: A Systematic Review on the Enablers and Barriers.
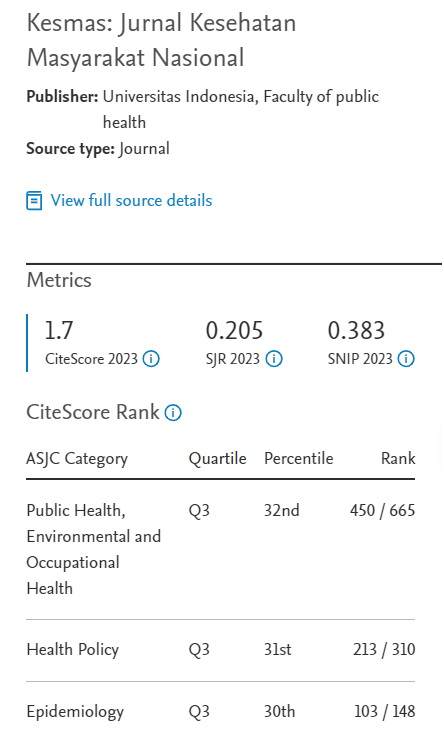
Kesmas.
2024;
19(4):
292-300
DOI: 10.21109/kesmas.v19i4.1343
Available at:
https://scholarhub.ui.ac.id/kesmas/vol19/iss4/9
Included in
Biostatistics Commons, Health Policy Commons, Health Services Research Commons, Public Health Education and Promotion Commons