Abstract
An effective way of learning about thalassemia, a complex public health issue with multiple perspectives, is through participating in research. This study used an inductive approach to presume the influencing factors of students' consent to participate in thalassemia research voluntarily. Nested in the preliminary stage of a research series on thalassemia, this study used a consecutive sampling to recruit 140 medical undergraduates. Their knowledge, experience, and attitude to thalassemia and the perception of self-quality life were assessed using self-administered questionnaires. Blood samples were drawn for carrier screening. Students' GPAs were collected from faculty records. Of 140 participants, only 123 had at least heard of thalassemia, and their data was used in the analysis. Most participants had fairly good but incomplete knowledge of inheritance patterns, antenatal screening, and thalassemia management. Premarital screening was known and received the most positive attitudes from participants. Inductively, academic performance and carrier status curiosity were presumed to influence students' consent to participate. With the limitation of an inductive approach, further study with a specific design is needed to closely investigate student perspectives on research and their drives to get involved.
References
1. Kohne E. Hemoglobinopathies: Clinical manifestations, diagnosis, and treatment. Dtsch Arztebl Int. 2011; 108 (31-32): 532-540. DOI: 10.3238/arztebl.2011.0532.
2. Wahidiyat PA, Sari TT, Rahmartani LD, et al. Thalassemia in Indonesia. Hemoglobin. 2022; 46 (1): 39-44. DOI: 10.1080/03630269.2021.2023565.
3. Kementerian Kesehatan Republik Indonesia. Pencegahan Thalassemia [Hasil Kajian HTA tahun 2009]. Jakarta: Kementerian Kesehatan Republik Indonesia; 2010.
4. Direktorat Pencegahan dan Pengendalian Penyakit Tidak Menular (P2PTM). Pedoman Pengendalian Penyakit Thalassemia di Fasilitas Kesehatan Tingkat Pertama. Jakarta: Kementerian Kesehatan Republik Indonesia; 2017.
5. Menteri Kesehatan Republik Indonesia. Keputusan Menteri Kesehatan RI Nomor HK.01.07/MENKES/1/2018 tentang Pedoman Nasional Pelayanan Kedokteran Tata Laksana Thalassemia. Jakarta: Kementerian Kesehatan Republik Indonesia; 2018.
6. Direktorat Pencegahan dan Pengendalian Penyakit Tidak Menular (P2PTM). Buku Pedoman Penyakit Tidak. Jakarta: Kementerian Kesehatan Republik Indonesia; 2019.
7. Sahiratmadja E, Seu MMV, Nainggolan IM, et al. Challenges in Thalassemia Carrier Detection in a Low Resource Setting Area of Eastern Indonesia: The Use of Erythrocyte Indices. Mediterr J Hematol Infect Dis. 2021; 13 (1): e2021003. DOI: 10.4084/MJHID.2021.003.
8. Widyawati W. Talasemia Penyakit Keturunan, Hindari dengan Deteksi Dini. Jakarta: Kementerian Kesehatan Republik Indonesia; 2022.
9. Indonesiabaik.id. Biaya besar talasemia di Indonesia. Jakarta: Indonesiabaik.id; 2019.
10. CNBC Indonesia. BPJS beri kemudahan untuk pasien Thalassemia & hemophilia. Jakarta: CNBC Indonesia; 2021.
11. Pratiwi S, Yuningsih A. Komunikasi persuasi Helper dalam menumbuhkan motivasi bagi penderita thalassemia. Pros Hub Masy Penelit SPeSIA. 2015; 1 (1): 142–152. DOI: 10.29313/.v0i0.200.
12. Marnis D, Indriati G, Nauli FA. Hubungan Tingkat Pengetahuan dengan Kualitas Hidup Anak Thalasemia. J Keperawatan Sriwijaya. 2018; 5 (2).
13. Tursinawati Y, Fuad W. Pengetahuan Pengaruhi Sikap dan Tindakan Mahasiswa terhadap Program Pencegahan Thalassemia di Indonesia. HIGEIA J Public Health Res Develop. 2018; 2 (4): 654-662. DOI: 10.15294/higeia.v2i4.25407.
14. Adiratna W, Udiyono A, Saraswati LD. Hubungan Pengetahuan dan Dukungan Sosial terhadap Skor Kepatuhan Minum Obat Kelasi Besi pada Pasien Thalassemia (Studi di RSUD Tidar Kota Magelang). J Kesehat Masy. 2020; 8 (1): 23-29. DOI: 10.14710/jkm.v8i1.25430.
15. Oktaria V, Kurniawati D. Hubungan Pengetahuan Talasemia Dengan Kepatuhan Keluarga Membawa Anak Menjalani Tranfusi Darah. J Ilmiah Kesehat. 2020; 9 (2): 94–97. DOI: 10.52657/jik.v9i2.1236.
16. Cuciati C, Mulyadi A, Abriyanto H, et al. Studi Korelasi Pengetahuan terhadap Sikap Mahasiswa Keperawatan dalam Pencegahan Generasi Thalasemia di Poltekkes Kemenkes Semarang Prodi DIII Keperawatan Tegal. Bhamada J Ilmu Teknol Kesehat. 2023; 14 (1): 1-5. DOI: 10.36308/jik.v14i1.438.
17. Saprudin N, Sudirman RM. Peningkatan Sikap dan Motivasi Orangtua tentang Perawatan Pasca Tranfusi pada Anak Thalasemia melalui Pemberian Komunikasi Informasi Edukasi Berbasis Audio Visual di Kabupaten Kuningan. J Nursing Pract Educ. 2020; 1 (1): 43-57.
18. Asa P, Indiastuti DN, Andarsini MR, et al. Empowering Thalassemia Patients and Family to Increase Public Knowledge on Thalassemia . J Pengabdian Masy. 2021; 7 (4): 228-233. DOI: 10.22146/jpkm.69349.
19. Himawan F, Suparjo S, Laksanano GS. Pemberdayaan Remaja dalam Upaya Sadar Bebas Thalasemia (Sabet). JABI J Abdimas Bhakti Indonesia. 2022; 3 (2): 76-81. DOI: 10.36308/jabi.v3i2.434.
20. Panigoro R, Prihatni D, Sribudiani Y, et al. Upaya menurunkan angka kejadian talasemia mayor melalui edukasi dan pemeriksaan darah pada acara donor darah: Menuju zero growth talasemia mayor di Indonesia. Dharmakarya J Apl Ipteks Masy. 2023; 12 (2): 182-188. DOI: 10.24198/dharmakarya.v12i2.37317.
21. Adiwijaya S, Aritonang DVA, Mashud M, et al. Empowerment Pattern for Thalassemia Patients in Dr. Soetomo Hospital Surabaya (Study of the Association of Parents with Thalassemia Indonesia, Surabaya). Budapest Int Res Critics Institute (BIRCI-Journal). 2018; 1 (4): 289-298. DOI: 10.33258/birci.v1i4.121.
22. Hijriani H. Pengaruh Psychoeducational Parenting Terhadap Kecemasan Orang Tua Yang Mempunyai Anak Penyandang Thalassemia Mayor di RSUD Majalengka. J Kampus STIKES YPIB Majalengka. 2017; V (2): 1-16.
23. Baroroh EZ. Intervensi Pelatihan Pengenalan Diri untuk Meningkatkan Self Esteem pada Remaja Penderita Thalassaemia. J Psikol Proyeksi. 2022; 17 (2): 13-24. DOI: 10.30659/jp.17.2.13-24.
24. Setiawati OR, Nurseha N, Pribadi T. Psikoedukasi terhadap kecemasan orang tua pasien yang menjalani pengobatan thalasemia mayor. Holistik J Kesehat. 2019; 13 (3): 225-232. DOI: 10.33024/hjk.v13i3.1369.
25. Widayanti CG, Ediati A, Tamam M, et al. Feasibility of preconception screening for thalassaemia in Indonesia: Exploring the opinion of Javanese mothers. Ethn Health. 2011; 16 (4-5): 483-499. DOI: 10.1080/13557858.2011.564607.
26. Cousins S, Blencowe NS, Blazeby JM. What is an invasive procedure? A definition to inform study design, evidence synthesis and research tracking. BMJ Open. 2019; 9: e028576. DOI: 10. 1136/bmjopen-2018-028576.
27. Khusun H, Yip R, Schultink W, et al. World Health Organization hemoglobin cut-off points for the detection of anemia are valid for an Indonesian population. J Nutr. 1999; 129 (9): 1669-1674. DOI: 10.1093/jn/129.9.1669.
28. Siswandari W, Rujito L, Indriani V, et al. Mentzer Index Diagnostic Value in Predicting Thalassemia Diagnosis. In: IOP Conference Series: Earth and Environmental Science; 2019. DOI: 10.1088/1755-1315/255/1/012004.
29. Maskoen AM, Reniarti L, Sahiratmadja E, et al. Shine & Lal index as a predictor for early detection of β-thalassemia carriers in a limited resource area in Bandung, Indonesia. BMC Med Genet. 2019; 20 (1): 136. DOI: 10.1186/s12881-019-0868-x.
30. Hamadeh N, Van Rompaey C, Metreau E. New World Bank country classifications by income level: 2021-2022. Washington, DC: New World Bank Blog; 2021.
31. Chakravorty S, Dick MC. Antenatal screening for haemoglobinopathies: Current status, barriers and ethics. Br J Haematol. 2019; 187 (4): 431-440. DOI: 10.1111/bjh.16188.
32. Cao A, Kan YW. The prevention of thalassemia. Cold Spring Harb Perspect Med. 2013; 3 (2): a011775. DOI: 10.1101/cshperspect.a011775.
33. Dahnil F, Mardhiyah A, Widianti E. Assessment of Supportive Care Needs in Parents of Children with Thalassemia. NurseLine J. 2017; 2 (1): 1-10. DOI: 10.19184/nlj.v2i1.5994.
34. Bell JS, Airaksinen MS, Lyles A, et al. Concordance is not synonymous with compliance or adherence. Br J Clin Pharmacol. 2007; 64 (5): 710-7111; author reply 711-713. DOI: 10.1111/j.1365-2125.2007.02971_1.x.
35. Haque ATME, Puteh FAB, Osman NLB, et al. Thalassaemia: Level of awareness among the future health care providers of Malaysia. J Chem Pharm Res. 2015; 7 (2): 896-902.
36. Alsuwaidi L, Powell L, Alhashmi D, et al. Volunteering among pre-clinical medical students: Study of its association with academic performance using institutional data. MedEdPublish. 2022; 12: 24. DOI: 10.12688/mep.19105.2.
37. Sahiratmadja E, Wijaya MA, Widjajakusuma A, et al. Pengetahuan Tentang Talasemia pada Mahasiswa Kedokteran dan Dokter Umum di Bandung serta Prevalensi Karir β-Thalassemia. J Indonesian Med Assoc. 2020; 70 (4): 48-58.
Recommended Citation
Wratsangka R , Adriani D , Tungka EX ,
et al.
The Influences of Medical Students' Consent to Participate in Thalassemia Research.
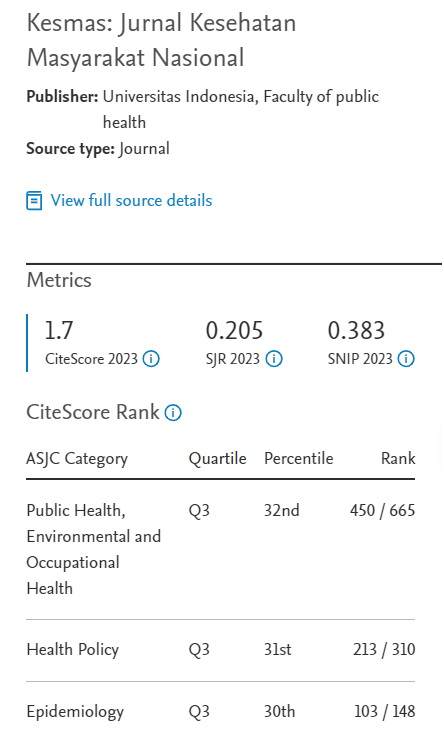
Kesmas.
2024;
19(2):
88-98
DOI: 10.21109/kesmas.v19i2.1099
Available at:
https://scholarhub.ui.ac.id/kesmas/vol19/iss2/3