Abstract
Infant anthropometry is an indicator of neonatal survival. This study aimed to determine the effects of maternal anthropometry on estimating infant anthropometry. This cross-sectional study on 173 pregnant women at Public Hospital X in Ternate, Indonesia, was conducted from August 2018 to March 2023. The eligible criteria were pregnant women aged ≥18 years, single pregnancy, and antenatal care (ANC) visits to the same hospital. The variables used included maternal anthropometric measurements (body weight, body height, third-trimester weight (TTW)), gestational weight gain (GWG), education, age, ANC visits, and gestational age at delivery (GAD). A logistic regression model was employed to estimate significant variables related to infant anthropometric measurements (birth weight, birth length, and head circumference). The results showed that TTW, GWG, ANC, and GAD had significantly affected birth weight. Bodyweight, height, and TTW also significantly affected birth length. In addition, only GAD significantly affected the head circumference. In multivariate analysis, TTW and GWG significantly affected birth weight. Furthermore, only body height and GAD affected the birth length. Maternal anthropometrics become important indicators for estimating birth weight and birth length.
References
1. Menteri Kesehatan Republik Indonesia. Peraturan Menteri Kesehatan Republik Indonesia Nomor 28 Tahun 2019 Tentang Angka Kecukupan Gizi yang Dianjurkan untuk Masyarakat Indonesia. Jakarta: Kementerian Kesehatan Republik Indonesia; 2019.
2. Tebbani F, Oulamara H, Agli A. Food diversity and nutrient intake during pregnancy in relation to maternal weight gain. Nutr Clin Metab. 2021; 35 (2): 93-99. DOI: 10.1016/j.nupar.2020.09.001
3. Onubugo CU, Egbuonu I, Ugochukwu EF, et al. The influence of maternal anthropometric characteristics on the size of term singleton South-East Nigerian newborn infants. Niger J Clin Pract. 2017; 20 (7): 852-859. DOI: 10.4103/njcp.njcp_308_16
4. Victora CG, Christian P, Vidaletti LP, et al. Revisiting maternal and child undernutrition in low-income and middle-income countries: Variable progress towards an unfinished agenda. Lancet. 2021; 397 (10282): 1388-1399. DOI: 10.1016/S0140-6736(21)00394-9
5. Kementerian Kesehatan Republik Indonesia. Profil Kesehatan Indonesia Tahun 2021. Jakarta: Kementerian Kesehatan Republik Indonesia; 2022.
6. National Population and Family Planning Board (BKKBN), Statistics Indonesia (BPS), Ministry of Health (Kemenkes), and ICF. Indonesia Demographic and Health Survey 2017. Jakarta, Indonesia: BKKBN, BPS, Kemenkes, and ICF; 2018.
7. Presiden Republik Indonesia. Rencana Pembangunan Jangka Menengah Nasional 2020-2024. Jakarta: Kementerian Sekretaris Negara; 2020.
8. Adawiyah AR, Djokosujono K, Alam N, et al. An effective method to predict low birth weight in Indonesia rural area. IJPHN. 2021; 2 (1): 12-19. DOI: 10.7454/ijphn.v2i1.5307.g1230
9. Djokosujono K, Putra WKY, Utari DM, et al. Prediction of low birth weight based on maternal third trimester weight among mothers at a maternal clinic in Jakarta, Indonesia. Media Gizi Indonesia. 2021; 16 (2): 106-110. DOI: 10.20473/mgi.v16i2.106-110
10. Jones I, Chandra PS, Dazzan P, et al. Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period. Lancet. 2014; 384 (ue 9956): 1789-1799. DOI: 10.1016/S0140-6736(14)61278-2
11. Stang J, Huffman LG. Position and Academy of Nutrition and Dietetics: Obesity, Reproduction, and Pregnancy Outcomes. J Acad Nutr Diet. 2016; 116 (4): 677-691. DOI: 10.1016/j.jand.2016.01.008
12. Hartiningrum I, Fitriyah N. Bayi berat lahir rendah (BBLR) di Provinsi Jawa Timur tahun 2012-2016. J Biom Kependuduk. 2018; 7 (2): 97-104. DOI: 10.20473/jbk.v7i2.2018.97-104
13. Mahumud RA, Sultana M, Sarker AR. Distribution and determination of low birth weight in developing countries. J Prev Med Public Health. 2017; 50 (1) : 18. DOI: 10.3961/jpmph.16.087
14. Gondwe A, Ashorn P, Ashorn U, et al. Pre-pregnancy body mass index (BMI) and maternal gestational weight gain are positively associated with birth outcomes in rural Malawi. PLoS ONE. 2018; 13 (10): e0206035. DOI: 10.1371/journal.pone.0206035
15. Kac G, Arnold CD, Matias SL, et al. Gestational weight gain and newborn anthropometric outcomes in rural Bangladesh. Matern Child Nutr. 2019; 15 (4): e12816. DOI: 10.1111/mcn.12816
16. Has EMM, Nursalam, Arief YS. Association between maternal factors and neonate anthropometry: A retrospective cross-sectional study. STRADA J Ilm Kes. 2021; 10 (1): 1024-1031. DOI: 10.30994/sjik.v10i1.757
17. Abide CY, Ergen EV, Kilicci C. Association between gestational weight gain and maternal and neonatal outcomes. East J Med. 2018; 23 (2): 115-120. DOI: 10.5505/ejm.2018.49389
18. Papazian T, Tayeh GA, Sibai D, et al. Impact of maternal body mass index and gestational weight gain on neonatal outcomes among healthy MiddleEastern females. PLoS ONE. 2017; 12 (7): e0181255. DOI: 10.1371/journal.pone.0181255
19. Morwani NP, Jain A, Sudhakar C. Effect of maternal age and gestational weight gain on anthropometry of newborn in semi urban area of Chhattisgarh, India. Int J Contemp Pediatr. 2019; 6 (6): 2374-2378. DOI: 10.18203/2349-3291.ijcp20194581
20. Liu X, Wang H, Yang L, et al. Associations between gestational weight gain and adverse birth outcomes: A population-based retrospective cohort study of 9 million mother-infant pairs. Front Nutr. 2022; 9: 811217. DOI: 10.3389/fnut.2022.811217
21. Baran J, Weres A, Czenczek-Lewandowska E, et al. Excessive gestational weight gain: Long-term consequences for the child. J Clin Med. 2020; 9: 3795. DOI: 10.3390/jcm9123795
22. Robbinson CA, Cohen AK, Rehkopf DH, et al. Pregnancy and post-delivery maternal weight changes and overweight in preschool children. Prev Med. 2014; 60: 77-82. DOI: 10.1016/j.ypmed.2013.12.018
23. Josey MJ, McCullough LE, Hoyo C, et al. Overall gestational weight gain mediates the relationship between maternal and child obesity. BMC Public Health. 2019; 19 (1): 1062. DOI: 10.1186/s12889-019-7349-1
24. Rönnberg AK. Gestational weight gain: Implication of an Antenatal lifestyle intervention [Dissertation]. Sweden: Urebro University; 2016. 61 p
25. Edi M, Chin YS, Woon FC, et al. Inadequate weight gain and exposure to second-hand smoke during pregnancy increase the risk low birth weight: A cross-sectional study among full-term infants. Int J Environ Res Public Health. 2021; 18 (3): 1068. DOI: 10.3390/ijerph18031068
26. Lamana A, Julia M, Dasuki D. Korelasi tinggi badan ibu dengan panjang badan bayi baru lahir di Kota Palu. J Kes Reprod. 2017; 4 (2): 103-108. DOI: 10.22146/jkr.35419
27. Abadi E, Putri LAR. Korelasi Antropometri Ibu Hamil dengan Panjang Badan Bayi Baru Lahir sebagai Prediktor Stunting. PROMOTIF J Kes Masy. 2020; 10 (02):167-172.
28. Dasantos PT, Dimiati H, Husnah. Hubungan berat badan lahir dan panjang badan lahir dengan stunting pada balita di Kabupaten Pidie. J Averrous. 2020; 6 (2): 29-43. DOI: 10.22146/jkr.35419
29. Zhang G, Bacelis J, Lengyei C, et al. Assessing the causal relationship of maternal height on birth size and gestational age at birth: A Mendelian randomization analysis. PLoS Med. 2015; 12 (8): e1001865. DOI: 10.1371/journal.pmed.1001865
30. Qurani RM, Karuniawaty TP, John RE, et al. Correlation between maternal factor and stunting among children of 6-12 months old in Central Lombok. JPH Recode. 2022; 5 (2): 107-116. DOI: 10.20473/jphrecode.v5i2.23525
31. Utami NH, Rachmalina R, Irawati A, et al. Short birth length, low birth weight and maternal short stature are dominant risks of stunting among children aged 0-23 months: Evidence from Bogor longitudinal study on child growth and development, Indonesia. Mal J Nutr. 2018; 24 (1): 11-23.
32. Manggala AK, Kenwa KWM, Kenwa MML, et al. Risk factors of stunting in children aged 24-59 months. Paediatrica Indonesiana. 2018; 58 (5): 205- 212. DOI: http://dx.doi.org/10.14238/pi58.5.2018.205-12
33. Derraik JGB, Lundgren M, Cutfield WS, et al. Maternal height and preterm birth: A study on 192,432 Swedish Women. PLoS One. 2016; 11 (4): e0154304. DOI: 10.1371%2Fjournal.pone.0154304
34. Nurwati Y, Hardinsyah H, Marliyati SA, et al. Potential maternal risk factors for low birth weight in Indonesia: A systematic review. J Gizi Pangan. 2023; 18 (3): 167-176. DOI: 10.25182/jgp.2023.18.3.167-176
35. Krismanita MD, Triyanti T, Syafiq A, et al. Determinants of the coexistence dual form of malnutrition in pairs of mother and child aged 6-59 months in Bogor District 2019. Kesmas. 2022; 17 (2): 129-135. DOI: 10.21109/kesmas.v17i2.5714
36. Christiani RE, Setyawati I, Yulihastuti DA. Morphology and skeletal development of rat (Rattus norvegicus) fetus after fed diets containing Calliandra calothyrsus leaf during gestation period. J Biol Udayana. 2016; 20 (2): 69-74. DOI: 10.24843/JBIOUNUD.2016.v20.i02.p05
37. Fitriani H, Setya A, Nurdiana P. Risk factors of maternal nutrition status during pregnancy to stunting in toddlers aged 12-59 months. J Kep Padjajaran. 2020; 8 (2): 175-183. DOI: 10.24198/jkp.v8i2.1305
Recommended Citation
Nurwati Y , Hardinsyah H , Marliyati SA ,
et al.
Effects of Maternal Anthropometry on Infant Anthropometry: A Cross-sectional Study at Public Hospital X in Ternate, Indonesia.
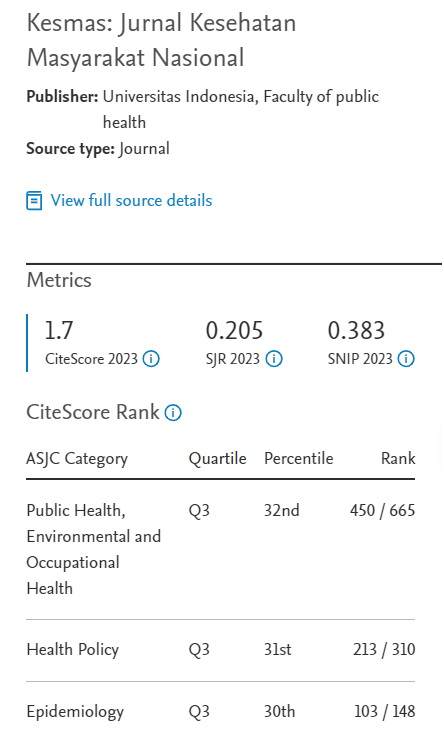
Kesmas.
2024;
19(1):
59-66
DOI: 10.21109/kesmas.v19i1.7336
Available at:
https://scholarhub.ui.ac.id/kesmas/vol19/iss1/8