Abstract
The COVID-19 pandemic disrupts rabies control activities in the community. A new approach is needed to control rabies during the COVID-19 pandemic through digital health interventions by conducting digital surveillance and education. This study aimed to determine key attitude indicators in controlling rabies during the COVID-19 pandemic. A cross-sectional study on 166 participants in Denpasar City with a total of 31 indicators measuring five variables: perceptions of the benefits of rabies control (6 indicators), perceptions of rabies risk (6 indicators), perceptions of obstacles to rabies control (5 indicators), perceptions of the need for technology (7 indicators), and attitudes toward rabies control (7 indicators) were analyzed using partial least square-structural equation modeling. The results revealed that 80.7% of participants owned a dog, and sources of rabies information were from social media (45%), the internet (33.7%), and rabies volunteers (33%). The model explained that perception of the benefits of rabies control and the need for technology had a direct effect on attitudes toward rabies control (p-value <0.001 and 0.015). In brief, perceived benefits and the need for technology influence attitudes toward rabies control during the COVID-19 pandemic.
References
1. Hampson K, Coudeville L, Lembo T, Sambo M, Kieffer A, et al. Estimating the Global Burden of Endemic Canine Rabies. PLoS Negl Trop Dis 2015; 9 (4): e0003709. DOI: 10.1371/journal.pntd.0003709
2. World Health Organization. WHO Expert Consultation on rabies: third report. Geneva: World Health Organization; 2018.
3. Direktorat Jenderal Pencegahan dan Pengendalian Penyakit. Laporan Kinerja Direktorat Pencegahan dan Pengendalian Penyakit Tular Vektor dan Zoonotik Tahun 2020. Jakarta: Kementerian Kesehatan Republik Indonesia; 2021.
4. Dewi APM, Riono P, Farid MN. Effects of Rabies Elimination Program on Rabies Cases in Bali, 2008-2015. In: The 1st International Conference of Global Health. 2018. KnE Life Sci. p. 62-73. DOI: 10.18502/kls.v4i1.1367
5. Putra AAG, Hampson K, Girardi J, Hiby E, Knobel D, Mardiana IW, et al. Response to a rabies epidemic, Bali, Indonesia, 2008-2011. Emerg Infect Dis. 2013; 19 (4): 648–651. DOI: 10.3201/eid1904.120380
6. Dinas Kesehatan Provinsi Bali. Sistem Kewaspadaan Dini dan Respon (SKDR) Berbasis Puskesmas di Provinsi Bali. Denpasar: Dinas Kesehatan Provinsi Bali; 2020.
7. Dinas Pertanian dan Ketahanan Pangan Provinsi Bali. Laporan Akuntabilitas Kinerja Pemerintah (LKjlP). Denpasar: Dinas Pertanian dan Ketahanan Pangan Provinsi Bali; 2021.
8. Raynor B, Díaz EW, Shinnick J, Zeggara E, Monroy Y, Mena C, et al. The impact of the COVID-19 pandemic on rabies reemergence in Latin America: The case of Arequipa, Peru. PLoS Negl Trop Dis. 2021; 15 (5): e0009414. DOI: 10.1371/journal.pntd.0009414
9. Townsend SE, Sumantra IP, Pudjiatmoko, Bagus GN, Brum E, Cleaveland S, et al. Designing Programs for Eliminating Canine Rabies from Islands: Bali, Indonesia as a Case Study. PLoS Negl Trop Dis. 2013; 7 (8): e2372. DOI: 10.1371/journal.pntd.0002372
10. Batan IW, Suatha IK. Faktor-Faktor yang Mendorong Kejadian Rabies pada Anjing di Desa-Desa di Bali (Factors Encouraging the Incidence of Rabies in Dogs in Villages in Bali). J Vet 2016; 17 (2): 274–279.
11. Widyastuti MDW, Bardosh KL, Sunandar, Basri C, Basuno E, Jatikusumah A, et al. On dogs, people, and a rabies epidemic: Results from a sociocultural study in Bali, Indonesia. Infect Dis Poverty. 2015; 4: 30. DOI: 10.1186/s40249-015-0061-1
12. Jeon S, Cleaton J, Meltzer MI, Kahn EB, Pieracci EG, Blanton JD, et al. Determining the post-elimination level of vaccination needed to prevent re-establishment of dog rabies. PLoS Negl Trop Dis. 2019; 13(2): e0007869. DOI: 10.1371/journal.pntd.0007869
13. Wallace RM, Undurraga EA, Gibson A, Pieracci EG, Gamble L, Blanton JD, et al. Estimating the effectiveness of vaccine programs in dog populations. Epidemiol Infect. 2019; 147: e247. DOI: 10.1017/S0950268819001158
14. Anuar H, Shah SA, Gafor AH, Mahmood MI, Ghazi HF. Usage of Health Belief Model (HBM) in health behavior: A systematic review. Mal J Med Heal Sci. 2020; 16 (Suppl 1): 201-209.
15. Morowatisharifabad MA, Karimi M, Jannati M. Utility of the health belief model to assess predictors of rabies preventive measures. J Educ Health Promot. 2014; 3: 62. DOI: 10.4103/2277-9531.134770
16. Suartha IN, Anthara MS, Dewi NMRK, Wirata IW, Mahardika IGNK, Dharmayudha AAGO, et al. Perhatian pemilik anjing dalam mendukung Bali bebas rabies. Bul Vet Udayana. 2014; 6 (1): 88–91.
17. Subrata M, Purnama SG, Utami AW, Agustina KK, et al. Peranan pemangku kepentingan dalam pengendalian rabies dengan pendekatan One Health Terintegrasi di Bali. J Kebijak Kesehat Indonesia. 2020; 9 (1): 20–32. DOI: 10.22146/jkki.54246
18. Kakang DM, Batan IW, Nindhia TS. Pemeliharaan Anjing oleh Masyarakat Kota Denpasar yang Berkaitan dengan Faktor Risiko Rabies. Indonesia Med Veterinus. 2017; 6 (2): 2477–6637.
19. Villanti AC, Johnson AL, Ilakkuvan V, Jacobs MA, Graham AL, Rath JM. Social media use and access to digital technology in US Young Adults in 2016. J Med Internet Res. 2017; 19 (6): e196 DOI: 10.2196/jmir.7303
20. Chen J, Wang Y. Social media use for health purposes: Systematic review. J Med Internet Res. 2021; 23 (5): e17917. DOI: 10.2196/17917
21. Wijayanti RP, Handayani PW, Azzahro F. Intention to seek health information on social media in Indonesia. Procedia Comput Sci. 2021; 197: 118–125. DOI: 10.1016/j.procs.2021.12.125
22. Huo J, Desai R, Hong YR, Turner K, Mainous AG. Bian J. Use of Social Media in Health Communication: Findings from the Health Information National Trends Survey 2013, 2014, and 2017. Cancer Control. 2019; 26 (1): 1073274819841442. DOI: 10.1177/1073274819841442
23. Ferguson AW, Muloi D, Ngatia DK, Kiongo W, Kimuyu DM, Webala PW, et al. Volunteer based approach to dog vaccination campaigns to eliminate human rabies: Lessons from Laikipia County, Kenya. PLoS Negl Trop Dis 2020; 14 (7): e0008260. DOI: 10.1371/journal.pntd.0008260
24. Xie T, Liu W, Anderson BD, Liu A, Gray GC. A system dynamics approach to understanding the One Health concept. PLoS One. 2017; 12 (9): e0184430. DOI: 10.1371/journal.pone.0184430
25. Destoumieux-Garzón D, Mavingui P, Boetsch G, Boissier J, Darriet F, Duboz P, et al. The one health concept: 10 years old and a long road ahead. Front Vet Sci. 2018; 5: 14. DOI: 10.3389/fvets.2018.00014
26. Mackenzie JS, Jeggo M. The one health approach-why is it so important? Trop Med Infect Dis. 2019; 4 (2): 88. DOI: 10.3390/tropicalmed4020088
27. Nadal D, Beeching S, Cleaveland S, Cronin K, Hampson K, Steenson R, et al. Rabies and the pandemic: Lessons for One Health. Trans R Soc Trop Med Hyg. 2022; 116 (3): 197-200. DOI: 10.1093/trstmh/trab123
28. Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver J. The Health Belief Model as an Explanatory Framework in Communication Research: Exploring Parallel, Serial, and Moderated Mediation. Health Commun. 2015; 30 (6): 566-576. DOI: 10.1080/10410236.2013.873363
29. Sesagiri Raamkumar A, Tan SG, Wee HL. Use of health belief modelbased deep learning classifiers for COVID-19 social media content to examine public perceptions of physical distancing: Model development and case study. JMIR Public Heal Surveill. 2020; 6 (3): e20493. DOI: 10.2196/20493
Recommended Citation
Purnama SG , Utami NA , Subrata M ,
et al.
Assessment of Rabies Control Attitudes During the COVID-19 Pandemic through Partial Least Square-Structural Equation Modeling.
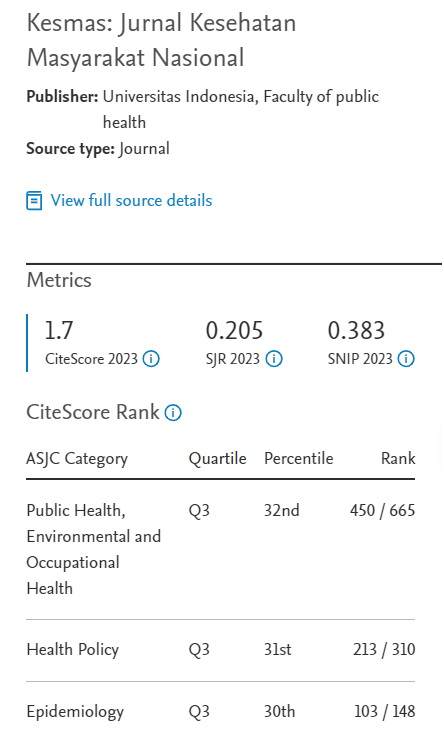
Kesmas.
2023;
18(2):
145-151
DOI: 10.21109/kesmas.v18i2.6890
Available at:
https://scholarhub.ui.ac.id/kesmas/vol18/iss2/9