Abstract
The COVID-19 pandemic has impacted the global decline in public health status. This study aimed to analyze the determinants of stunting in the under-five in three municipalities in the Special Capital Region of Jakarta, Indonesia. A cross-sectional study was conducted in August-December 2020 with 460 pairs of mothers and children selected by simple random sampling. Stunting was measured using a conventional anthropometric index (length/height-for-age), and anthropometric failure was measured using the Composite Index of Anthropometric Failure. The prevalence of stunting, underweight, and wasting was 41.5%,35%, and 19.8%, respectively, and 62% of the under-five experienced anthropometric failure. The dominant factor associated with stunting was immunization record (p-value = 0.011; AOR = 2.360; 95%CI = 1.218–4.573). Children who did not receive complete basic immunization were at a 2.4 times greater risk of stunting than children who received complete basic immunization. The dominant factors associated with underweight, wasting, and anthropometric failure were the father's educational level, mother's occupation, and balanced nutrition practice. Increasing coverage of complete basic immunization, improving balanced nutrition practices and socioeconomic conditions is necessary to prevent undernutrition, especially stunting.
References
1. Ekholuenetale M, Barrow A, Ekholuenetale CE, Tudeme G. Impact of stunting on early childhood cognitive development in Benin: evidence from Demographic and Health Survey. Egyptian Pediatric Association Gazette. 2020; 68 (1): 31.
2. Casadei K, Kiel J. Anthropometric measurement. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
3. UNICEF, WHO, World Bank. Levels and trends child malnutrition: key findings of the 2020 edition of the joint child malnutrition estimate. Geneva: World Health Organization; 2020.
4. Murarkar S, Gothankar J, Doke P, Pore P, Lalwani S, Dhumale G, et al. Prevalence and determinants of undernutrition among under-five children residing in urban slums and rural area, Maharashtra, India: a community-based cross-sectional study. BMC Public Health. 2020; 20 (1): 1559.
5. Chowdhury MRK, Khan HTA, Mondal MNI. Differences in the socio - demographic determinants of undernutrition in children aged2021; 198: 37–43.
6. Kementerian Kesehatan Republik Indonesia. Buku Saku Hasil Survei Status Gizi (SSGI) Tingkat Nasional, Provinsi, dan Kabupaten/Kota Tahun 2021. Jakarta: Kementerian Kesehatan Republik Indonesia; 2021.
7. Widyaningsih V, Mulyaningsih T, Rahmawati FN, Adhitya D. Determinants of socioeconomic and rural-urban disparities in stunting: evidence from Indonesia. Rural Remote Health. 2022; 22 (1): 7082.
8. Ayuningtyas D, Hapsari D, Rachmalina R, Amir V, Rachmawati R, Kusuma D. Geographic and socioeconomic disparity in child undernutrition across 514 districts in Indonesia. Nutrients. 2022; 14 (4): 843.
9. Siswati T, Hoekstra T, Kusnanto H. Stunting among children Indonesian urban areas: What is the risk factors? Jurnal Gizi dan Dietetik Indonesia (Indonesian Journal of Nutrition and Dietetics). 2020; 8 (1): 1–8.
10. Dayuningsih, Permatasari TAE, Supriyatna N. Pengaruh pola asuh pemberian makan terhadap kejadian stunting pada balita. Jurnal Kesehatan Masyarakat Andalas. 2020; 14 (2): 3–11.
11. Kementerian Kesehatan Republik Indonesia. Kuesioner Individu Riset Kesehatan Dasar 2018. Jakarta: Kementerian Kesehatan Republik Indonesia; 2018.
12. Permatasari TAE, Chadirin Y. Assessment of undernutrition using the composite index of anthropometric failure (CIAF) and its determinants: a cross-sectional study in the rural area of the Bogor District in Indonesia. BMC Nutr. 2022; 8 (1): 133.
13. Sserwanja Q, Kamara K, Mutisya LM, Musaba MW, Ziaei S. Rural and urban correlates of stunting among under-five children in Sierra Leone: a 2019 nationwide cross-sectional survey. Nutr Metab Insights. 2021; 14: 11786388211047056.
14. Das S, Chanani S, Shah More N, Osrin D, Pantvaidya S, Jayaraman A. Determinants of stunting among children under 2 years in urban informal settlements in Mumbai, India: evidence from a household census. J Health Popul Nutr. 2020; 39 (1): 10.
15. Wali N, E Agho K, Renzaho AMN. Wasting and associated factors among children under 5 years in five South Asian Countries (2014– 2018): analysis of demographic health surveys. Int J Environ Res Public Health. 2021; 18 (9): 4578.
16. Frimawaty E, Kamiluddin MM. Living room ventilation and urban environmental health case in DKI Jakarta. Journal of Environmental Science and Sustainable Development. 2020; 3 (1): 195–209.
17. Damanik S, Wanda D, Hayati H. Feeding practices for toddlers with stunting in Jakarta: a case study. Pediatr Rep. 2020; 12 (Suppl 1): 8695.
18. Fajariyah RN, Hidajah AC. Correlation between immunization status and mother’s height, and stunting in children 2–5 years in Indonesia. Jurnal Berkala Epidemiologi. 2020; 8 (1): 89-96.
19. Ferreira HDS, Albuquerque GT, Santos TRD, Barbosa RL, Cavalcante AL, Duarte LEC, et al. Stunting and overweight among children in Northeast Brazil: Prevalence, trends (1992-2005-2015) and associated risk factors from repeated cross-sectional surveys. BMC Public Health. 2020; 20 (1): 736.
20. Shinsugi C, Mizumoto A. Associations of nutritional status with full immunization coverage and safe hygiene practices among Thai children aged 12–59 months. Nutrients. 2021; 14 (1): 34.
21. Islam MS, Biswas T. Prevalence and correlates of the composite index of anthropometric failure among children under 5 years old in Bangladesh. Matern Child Nutr. 2020; 16 (2): e12930.
22. Tusting LS, Bradley J, Bhatt S, Gibson HS, Weiss DJ, Shenton FC, et al. Environmental temperature and growth faltering in African children: a cross-sectional study. The Lancet Planetary Health. 2020; 4 (3): e116–23.
23. Huriah T, Handayani P, Sudyasih T, Susyanto BE. The determinant factors of stunting among children in urban slums area, Yogyakarta, Indonesia. Open Access Maced J Med Sci. 2021; 9 (T4): 1–5.
24. Headey D, Hirvonen K, Hoddinott J. Animal sourced foods and child Stunting. Am J Agric Econ. 2018; 100 (5): 1302–19.
25. Vollmer S, Bommer C, Krishna A, Harttgen K, Subramanian SV. The association of parental education with childhood undernutrition in low- and middle-income countries: comparing the role of paternal and maternal education. Int J Epidemio. 2017; 46 (1): 312–23.
26. Chowdhury TR, Chakrabarty S, Rakib M, Saltmarsh S, Davis KA. Socio-economic risk factors for early childhood underweight in Bangladesh. Global Health. 2018; 14 (1): 54.
27. Ketema B, Bosha T, Feleke FW. Effect of maternal employment on child nutritional status in Bale Robe Town, Ethiopia: a comparative cross-sectional analysis. J Nutr Sci. 2022; 11: e28.
28. Fadare O, Amare M, Mavrotas G, Akerele D, Ogunniyi A. Mother’s nutrition-related knowledge and child nutrition outcomes: empirical evidence from Nigeria. PloS one. 2019; 14 (2): e0212775.
29. Seboka BT, Hailegebreal S, Yehualashet DE, Demeke AD. Tracking progress in anthropometric failure among under-five children in Ethiopia: a geospatial and multilevel analysis. Arc Public Health. 2021; 79 (1): 103.
30. Dasgupta A, Shree N, Paul B, Bandyopadhyay L, Roy S, Maurya N, et al. Burden of undernutrition among children of 12-59 months living in a slum of Kolkata: a cross-sectional study. Int J Community Med Public Health. 2021; 8 (8): 3927–33.
Recommended Citation
Permatasari TA , Chairunnisa C , Djarir H ,
et al.
The Determinants of Stunting in the Under-five in Three Municipalities in the Special Capital Region of Jakarta.
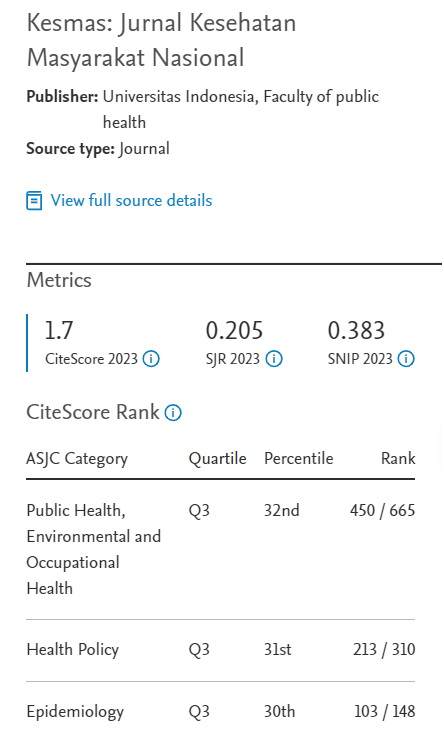
Kesmas.
2023;
18(1):
32-40
DOI: 10.21109/kesmas.v18i1.6405
Available at:
https://scholarhub.ui.ac.id/kesmas/vol18/iss1/5
Included in
Biostatistics Commons, Environmental Public Health Commons, Epidemiology Commons, Health Policy Commons, Health Services Research Commons, Nutrition Commons, Occupational Health and Industrial Hygiene Commons, Public Health Education and Promotion Commons, Women's Health Commons