Abstract
This study aimed to investigate the perspectives of reproductive health education among Javanese parents of children aged 9-11 years. This cross-sectional study was conducted with 12,306 parents in Semarang City, Central Java Province, Indonesia, using a purposive sampling technique. Some parents agreed that reproductive health education at home was unnecessary (29.5%), taboo (45%), difficult (73.1%), and awkward (41.5%). Most parents (72.7%) were not transparent in providing reproductive health information to their children by using other terms to name the genitals, considering the politeness aspect. Good practices of providing reproductive health information are slightly more common in mothers (54.2%), unemployed parents (52.9%), those with a higher education level (69.5%), and those with a family income above the regional minimum wage (59.8%). As many as 76.9% of parents intensely monitor their children; however, 60.63% of parents have poor communications with their children. Parents believe that reproductive health information is essential for their children, but parents find the topic difficult with their children due to taboos and awkward feelings. Accordingly, the Indonesian Ministry of Health should empower parents to discuss reproductive health issues with their children openly.
References
1. Ajayi AI, Odunga SA, Oduor C, Ouedraogo R, Ushie BA, Wado YD. “I was tricked”: understanding reasons for unintended pregnancy among sexually active adolescent girls. Reprod Health. 2021; 18 (1): 19.
2. Bearak J, Popinchalk A, Alkema L, Sedgh G. Global, Regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014: estimates from a Bayesian Hierarchical model. Lancet Glob Heal. 2018; 6 (4): e380–9.
3. Ganatra B, Gerdts C, Rossier C, Johnson BR Jr, Tunçalp Ö, et al. Global, regional, and subregional classification of abortions by safety, 2010–14: estimates from a Bayesian hierarchical model. Lancet. 2017; 390 (10110): 2372–81.
4. Singh S, Shekhar C, Acharya R, Moore AM, Stillman M, Pradhan MR, et al. The incidence of abortion and unintended pregnancy in India, 2015. Lancet Glob Heal. 2018; 6 (1): 111–20.
5. Ocviyanti D, Dorothea M. Aborsi di Indonesia. J Indones Med Assoc. 2018; 68 (6): 213–5.
6. Pusat Penelitian dan Pengembangan Upaya Kesehatan Masyarakat. Perilaku berisiko kesehatan pada pelajar SMP dan SMA di Indonesia. Pusat Penelitian dan Pengembangan Upaya Kesehatan Masyarakat; 2016.
7. Kementerian Kesehatan Republik Indonesia. Situasi kesehatan reproduksi remaja. Jakarta; Pusat Data dan Informasi Kementerian Kesehatan Republik Indonesia; 2015.
8. Badan Kependudukan dan Keluarga Berencana Nasional. Survei Demografi dan kesehatan Indonesia 2017: Buku Remaja. Jakarta; Badan Kependudukan dan Keluarga Berencana Nasional; 2018.
9. Sasongko AJ. Tingginya kehamilan remaja tuntut PKBI Jateng susun program kerja 2015-2018. PKBI Daerah Jawa Tengah; 2019.
10. Wahab A, Wilopo SA, Hakimi M, Ismail D. Declining age at menarche in Indonesia: a systematic review and meta-analysis. Int J Adolesc Med Health. 2018; 32 (6).
11. Gayatri S, Shaluhiyah Z, Indraswari R. Faktor-faktor yang berhubungan dengan frekuensi akses pornografi dan dampaknya terhadap perilaku seksual pada remaja di Kota Bogor. J Kesehat Masy. 2020; 8 (3): 410–9.
12. Wulandari S. Perilaku seksual pranikah berisiko terhadap kehamilan tidak diinginkan pada remaja SMKN Tandun Kabupaten Rokan Hulu. J Matern Neonatal. 2016; 4 (1): 74–84.
13. Wanufika I, Sumarni S, Ismail D. Komunikasi orang tua tentang seksualitas terhadap perilaku seksual pranikah remaja. Ber Kedokt Masy. 2017; 33 (10): 495–500.
14. Badan Kependudukan dan Keluarga Berencana Nasional. Survei demografi dan kesehatan Indonesia 2017: kesehatan reproduksi remaja (indikator utama). Jakarta: Badan Kependudukan Keluarga Berencana Nasional; 2018.
15. Rusady IK, Shaluhiyah Z, Husodo BT. Analisis kebutuhan pendidikan kesehatan reproduksi pada diswa SMP di wilayah Kecamatan Pedurungan Semarang. J Kesehat Masy. 2017; 5 (5): 1010–20.
16. Mohammad-Esmaeil M, Rejaei L, Jonidi AJ, Ardalan G, Dorouzi J, Rezaei N, et al. Priorities in health education needs of youth based on needs assessment and stakeholder involvement, in areas covered by the Health Departments of Iran University of Medical Sciences. J Educ Community Heal. 2016; 3: 51–7.
17. Indraswari R, Shaluhiyah Z, Widjanarko B, Suryoputro A. Factors of mothers’ hesitation in discussing reproductive health. Int J Public Heal Sci. 2021; 10 (4): 801–6.
18. Lange A, Blonk R, Wiers RW. Assessment: the parent-child interaction questionnaire, PACHIQ. Clin Psychol Psychother. 1998; 5(3): 187–98.
19. Fischer AL, O’Rourke N, Thornton WL. Age differences in cognitive and affective theory of mind: concurrent contributions of neuro cog - nitive performance, sex, and pulse pressure. J Gerontol B Psychol Sci Soc Sci. 2017; 72 (1): 71–81.
20. Correia R, Barroso J, Nieto A. Age-related cognitive changes: the importance of modulating factors. J Geriatr Med Gerontol. 2018; 4 (2): 1–10.
21. Sigiro AN. Care Economy and the burden of housewives’ work in Indonesia. J Peremp. 2018; 23 (4): 249.
22. Navickienė V, Sederevičiūtė-Pačiauskienė Ž, Valantinaitė I, Žilinskaitė-Vytienė V. The relationship between communication and education through the creative personality of the teacher. Creat Stud. 2019; 12 (1): 49–60.
23. Obaki SO. Impact of classroom environment on children’s social behavior. Int J Educ Pract. 2017; 5 (1): 1–7.
24. Dávila SPE, Champion JD, Monsiváis MGM, Tovar M, Arias MLF. Mexican adolescents’ self-reports of parental monitoring and sexual communication for prevention of sexual risk behavior. J Pediatr Nurs. 2017; 35: 83–9.
25. Handayani S. Faktor-faktor yang mempengaruhi kejadian kehamilan tidak diinginkan pada remaja di Kelurahan Balecatur Gampingan Sleman Yogyakarta. J Kesehat Samudra Ilmu. 2016; 7 (1).
26. Green LW, Kreuter MW. Health promotion: planning an educational and environmental approach. 2nd ed. CA: Mayfield; 1991.
27. Shin H, Lee JM, Min JY. Sexual knowledge, sexual attitudes, and perceptions and actualities of sex education among elementary school parents. Child Heal Nurs Res. 2019; 25 (3): 312–23.
28. Robinson KH, Smith E, Davies C. Responsibilities, tensions and ways forward: parents’ perspectives on children’s sexuality education. Sex Educ. 2017; 17 (3): 333–47.
29. Runcan R, Bahnaru A. Sex education revisited: school-based sex education. Analele Univ din Craiova. 2019; 18 (1): 1–7.
30. Khoshsaligheh M, Ameeri S, Mehdizadkhani M. A Socio-cultural study of taboo rendition in Persian fansubbing: an issue of resistance. Lang Intercult Commun. 2018; 18 (6): 663–80.
31. Robati FZNN, Zand F. Translation of taboos: the absolutely true diary of a part-time Indian. Int J Appl Linguist English Lit. 2018; 7 (3): 35– 40.
32. Azira N, Abdullah FB, Muda SM, Zain NM. The role of parents in providing sexuality education to their children. Makara J Heal Res. 2020; 24 (3): 157–63.
Recommended Citation
Widjanarko B , Indraswari R , Kusumawati A ,
et al.
Perspectives on Reproductive Health Education among Javanese Parents.
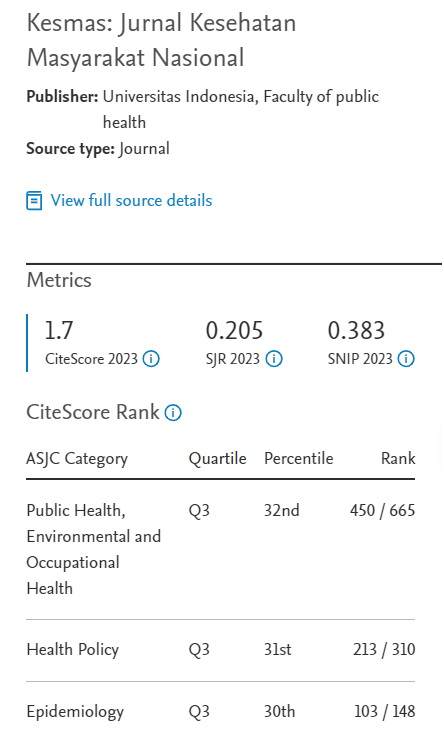
Kesmas.
2022;
17(3):
212-219
DOI: 10.21109/kesmas.v17i3.5893
Available at:
https://scholarhub.ui.ac.id/kesmas/vol17/iss3/8
Included in
Biostatistics Commons, Environmental Public Health Commons, Epidemiology Commons, Health Policy Commons, Health Services Research Commons, Nutrition Commons, Occupational Health and Industrial Hygiene Commons, Public Health Education and Promotion Commons, Women's Health Commons