Abstract
The Indonesian Government established a social distancing policy to prevent COVID-19 transmission. However, this implementation will be ineffective without the compliance of the people. This study aimed to analyze the relationship between public perception and obedience with social distancing in terms of the variables based on the Health Belief Model. This study used a cross-sectional design with a population of Daerah Khusus Ibukota (DKI) Jakarta’s indigenes within the productive age of 15-64 years. The sample comprised 408 participants, with the independent variables of sociodemographics (age, gender, occupation, and education) and health beliefs (perceived susceptibility, severity, benefits, barriers, and self-efficacy). Meanwhile, obedience to social distancing was the dependent variable. Data were obtained through an online questionnaire and evaluated with the bivariate and multivariate analysis using Chi-square and logistic regression tests. Gender (OR = 2.327; 95% CI = 1.404-3.857) and perceived self-efficacy (OR = 2.609; 95% CI = 1.726-3.945) were significantly related to social distancing obedience. Meanwhile, no statistical correlation (p-value>0.05) was found with sociodemographics, perceived susceptibility, severity, benefits, and barriers. The males with low self-efficacy were more likely to disobey the social distancing policies. The individual’s self-efficacy perception increased with their level of obedience to social distancing policies.
References
1. Olney AM, Smith J, Sen S, Thomas F, Unwin HJT. Estimating the effect of social distancing interventions on COVID-19 in the United States. medRxiv; 2020.
2. Herdiana D. Social distancing: Indonesian policy response to the Corona virus disease 2019 (COVID-19). Jurnal Ilmu Administrasi: Media Pengembangan Ilmu dan Praktek Administrasi. 2020; 17 (1): 93–110.
3. Australian Government Department of Health. Coronavirus disease (COVID-19) social distancing guidance; 2020.
4. Satuan Tugas Penanganan COVID-19. Peta sebaran COVID-19; 2021.
5. Funk S, Gilad E, Watkins C, Jansen VAA. The spread of awareness and its impact on epidemic outbreaks. Proceedings of the National Academy of Sciences. 2009; 106 (16): 6872–7.
6. Rivers C, Inglesby T. What is social distancing and how can it slow the spread of COVID-19? Hub; 2020.
7. Pearce K. What is social distancing and how can it slow the spread of COVID-19? Hub; 2020.
8. Bavel J, Baicker K, Boggio P, Capraro V, Cichocka A, Cikara M, et al. Using social and behavioural science to support COVID-19 pandemic response. Nature Human B ehaviour. 2020; 4 (5): 460–71.
9. World Health Organization. What is social distancing and how can it slow the spread of COVID-19? Hub; 2020.
10. Zhang Y, Jiang B, Yuan J, Tao Y. The impact of social distancing and epicenter lockdown on the COVID-19 epidemic in mainland China: a data-driven SEIQR model study. medRxiv; 2020.
11. Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N, et al. Estimates of the severity of COVID-19 disease. medRxiv; 2020.
12. Taeyong L, Hee-Dae K, Jeehyun L. The effect of control measures on COVID-19 transmission in South Korea. PLoS ONE. 2021; 16 (3): e0249262.
13. Nasir EF, Yagoub HMA, Alhag AK. Study of the Sudanese perceptions of COVID-19: applying the health belief model. medRxiv; 2020.
14. Nurina L. Kajian empiris tentang kepatuhan wajib pajak orang pribadi di Kota Surakarta; 2010.
15. Kementerian Kesehatan Republik Indonesia. Peraturan Menteri Kesehatan Republik Indonesia Nomor 9 Tahun 2020 Tentang Pedoman Pembatasan Sosial Berskala Besar Dalam Rangka Percepatan Penanganan Corona Virus Disease 2019 (COVID-19); 2020.
16. Gubernur DKI Jakarta. Peraturan Gubernur Daerah Khusus Ibukota Jakarta Nomor 3 Tahun 2021 Tentang Peraturan Pelaksanaan Peraturan Daerah Nomor 2 Tahun 2020 Tentang Penanggulangan Corona Virus Disease 2019; 2021.
17. Rosenstock IM. The health belief model and preventive health behavior. Health Education Monographs. 1974; 2 (4): 354-86.
18. Tang CSK, Wong CY. Factors influencing the wearing of facemasks to prevent the severe acute respiratory syndrome among adult Chinese in Hong Kong. Preventive Medicine. 2004; 39 (6): 1187–93.
19. Afrianti N, Rahmiati C. Faktor-faktor yang mempengaruhi kepatuhanmasyarakat terhadap protokol kesehatan Covid-19. Jurnal Ilmiah Permas: Jurnal Ilmiah STIKES Kendal. 2021; 11 (1): 113–24.
20. Vlassoff C. Gender Differences in determinants and consequences of health and illness. Journal of Health, Population, and Nutrition. 2007; 25 (1): 47-61.
21. Larasaty P. Faktor yang berpengaruh terhadap kepatuhan masyarakat pada protokol kesehatan dalam mencegah penyebaran COVID-19. Seminar Nasional Official Statistics. 2020; 2020 (1): 45–54.
22. Vadaparampil ST, Champion VL, Miller TK, Menon U, Skinner CS. Using the health belief model to examine differences in adherence to mammography among African-American and Caucasian women. Journal of Psychosocial Oncology. 2008; 21 (4): 59–79.
23. Shahnazi H, Ahmadi-Livani M, Pahlavanzadeh B, Rajabi A, Hamrah MS, Charkazi A. Assessing preventive health behaviors from COVID19: a cross sectional study with health belief model in Golestan Province, Northern of Iran. Infectious Diseases of Poverty. 2020; 9 (1): 1–9.
24. Badan Pusat Statistik DKI Jakarta. Rata-rata upah/gaji bersih sebulan pekerja informal menurut Kabupaten/Kota dan lapangan pekerjaan utama (rupiah) di Provinsi DKI Jakarta 2018-2020; 2020.
Recommended Citation
Widyamurti W , Sitorus EB , Susanna D ,
et al.
Public Perception and Obedience with Social Distancing Policies during the COVID-19 Pandemic in Jakarta, Indonesia.
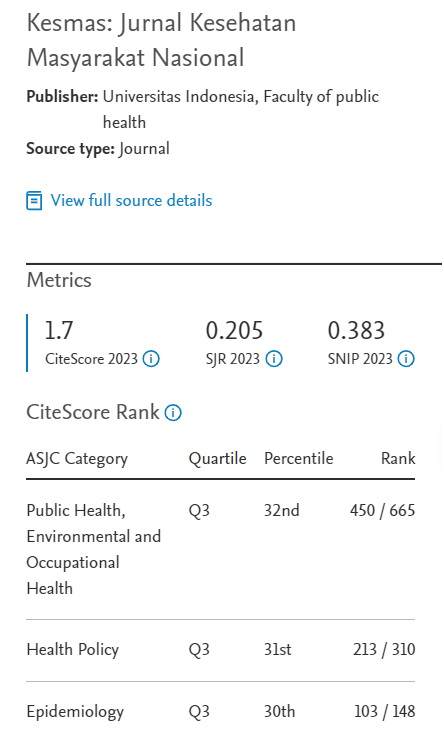
Kesmas.
2022;
17(1):
74-80
DOI: 10.21109/kesmas.v17i1.5430
Available at:
https://scholarhub.ui.ac.id/kesmas/vol17/iss1/11
Included in
Biostatistics Commons, Environmental Public Health Commons, Epidemiology Commons, Health Policy Commons, Health Services Research Commons, Nutrition Commons, Occupational Health and Industrial Hygiene Commons, Public Health Education and Promotion Commons, Women's Health Commons