Abstract
The broad availability of sugar-sweetened beverages (SSBs) in the Indonesian market is increasing consumption. It, combined with escalating incidence and prevalence of diabetes and related non-communicable diseases (NCDs), and the ongoing debate on policies, has called for a comprehensive review as described in this study. Data was compiled from various sources but mainly gathered from the reported or published documents because of no direct access to the necessary data set. The lack of studies that assessed the direct relationship between SSB consumption and health outcomes in the Indonesian context also became a strong reason for the preparation of this review to highlight important points for further research, academic reviews, and debates on empiric policies to control sugar consumption at the population level. Sociocultural factors were an apparent and crucial determinant of the sweetness preferences of mainstream Indonesians. They were not capitalized in the available documents and should be embraced in future health promotional measures. Given the high contribution of carbohydrates and sugar to total energy intake in the Indonesian diet, it is pertinent to control the increasing trend of SSBs consumption through interventions on both the supply and demand sides.
References
1. Bleich SN, Vercammen KA. The negative impact of sugar-sweetened beverages on children’s health: an update of the literature. BMC Obes. 2018; 5 (1): 6.
2. Amies-Cull B, Briggs ADM, Scarborough P. Estimating the potential impact of the UK government’s sugar reduction programme on child and adult health: modelling study. BMJ. 2019; 365: l1417.
3. Colchero MA, Popkin BM, Rivera JA, Ng SW. Beverage purchases from stores in Mexico under the excise tax on sugar sweetened beverages: observational study. BMJ. 2016; 352: h6704.
4. Veerman JL, Sacks G, Antonopoulos N, Martin J. The impact of a tax on sugar-sweetened beverages on health and health care costs: a mo - del ling study. PLoS One. 2016; 11 (4): 1–10.
5. Eyles H, Ni Mhurchu C, Nghiem N, Blakely T. Food pricing strategies, population diets, and noncommunicable disease: a systematic review of simulation studies. PLoS Med. 2012; 9 (12): e1001353.
6. World Health Organization. Fiscal policies for diet and the prevention of noncommunicable diseases: technical meeting report. Geneva: WHO; 2015.
7. World Health Organization. Handbook for guideline development 2nd ed. Geneva: WHO; 2014.
8. Ventura AK, Mennella JA. Innate and learned preferences for sweet taste during childhood. Curr Opin Clin Nutr Metab Care. 2011; 14 (4): 379–84.
9. Lenoir M, Serre F, Cantin L, Ahmed SH. Intense sweetness surpasses cocaine reward. PLoS One. 2007; 2 (8).
10. Mennella JA, Jagnow CP, Beauchamp GK. Prenatal and postnatal flavor learning by human infants. Pediatrics. 2001; 107 (6): e88.
11. Liem DG, De Graaf C. Sweet and sour preferences in young children and adults: role of repeated exposure. Physiol Behav. 2004; 83 (3): 421–9.
12. Liem DG, Mennella JA. Sweet and sour preferences during childhood: role of early experiences. Dev Psychobiol. 2002; 41 (4): 388–95.
13. Haughton CF, Waring ME, Wang ML, Rosal MC, Pbert L, Lemon SC. Home matters: adolescents drink more sugar-sweetened beverages when available at home. J Pediatr. 2018; 202: 121–8.
14. Pinard CA, Davy BM, Estabrooks PA. Beverage intake in low-income parent–child dyads. Eat Behav. 2011; 12 (4): 313–6.
15. Fiorito LM, Marini M, Mitchell DC, Smiciklas-Wright H, Birch LL. Girls’ early sweetened carbonated beverage intake predicts different patterns of beverage and nutrient intake across childhood and adolescence. J Am Diet Assoc. 2010; 110 (4): 543–50.
16. Lora KR, Hubbs-Tait L, Ferris AM, Wakefield D. African-American and hispanic children’s beverage intake: differences in associations with desire to drink, fathers’ feeding practices, and weight concerns. Appetite. 2016; 107: 558–67.
17. Bogart LM, Elliott MN, Ober AJ, Klein DJ, Hawes-Dawson J, Cowgill BO, et al. Home sweet home: parent and home environmental factors in adolescent consumption of sugar-sweetened beverages. Acad Pediatr. 2017; 17 (5): 529–36.
18. Federal Research Division. Indonesia: a country study. 6th ed. Frederik H, Worden RL, editors. Library of Congress; 2011.
19. Seri Buku Tempo. Antropologi kuliner nusantara (The anthropology of culinary archipelago). 1th ed. Jakarta: PT. Gramedia; 2015.
20. Buahpena FIB. Wadah karya FIB UGM; 2015.
21. Wahyuni S, Sinuraya JF. Industri dan perdagangan gula di Indonesia : pembelajaran dari kebijakan zaman penjajahan – sekarang (Sugarcane industry and trade : lesson learned from the applied policies during the colonial era up until this period). Forum penelitian Agro Ekonomi. 2009; 27 (2): 151-67.
22. Nitisastro W. Population trends in Indonesia. Equinox Publishing; 2006.
23. Gooszen H. A demographic history of the Indonesian Archipelago 1880-1942. The Netherlands: KITLV Press; 1999.
24. Subiyanto H. Peta Pabrik Gula Indonesia; 2015.
25. Asosiasi Industri Minuman Ringan (The Association of Soft Drink). Kinerja dan tantangan industri minuman ringan; 2020.
26. Laksmi PW, Morin C, Gandy J, Moreno LA, Kavouras SA, Martinez H, et al. Fluid intake of children, adolescents and adults in Indonesia: results of the 2016 Liq.In7 national cross-sectional survey. Eur J Nutr2018; 57(3): 89–100.
27. World Health Organization. Guideline: sugars intake for adults and children. World Health Organization; 2015.
28. Kementerian Kesehatan Republik Indonesia. Peraturan Menteri Kesehatan Republik Indonesia nomor 30 tahun 2013 tentang pencantuman kandungan gula, garam, dan lemak serta pesan kesehatan untuk pangan olahan dan pangan siap saji; 2013.
29. Badan Pengawas Obat dan Makanan Republik Indonesia. Peraturan Kepala Badan Pengawasan Obat dan Makanan Republik Indonesia nomor 22 tahun 2019 tentang informasi nilai gizi pada label pangan olahan; 2019.
30. Badan Penelitian dan Pengembangan Kesehatan Republik Indonesia. Studi diet total : survei konsumsi makanan individu. Jakarta; 2014.
31. Daeli WAC, Nurwahyuni A. Determinan sosial ekonomi konsumsi minuman berpemanis di Indonesia : analisis data susenas 2017. Jurnal Ekonomi Kesehatan Indonesia. 2019; 4(1): 1-11.
32. Ministry of Health of Indonesia. Basic Health Research 2018. Badan Penelitian dan Pengembangan Kesehatan. Jakarta; 2018.
33. Verakadita F. Minuman ringan dengan pemanis gula (MRDPG): pola konsumsi dan hubungannya dengan obesitas pada anak sekolah usia 10-12 tahun (studi kasus di sekolah Al-Azhar Rawamamangun Jakarta Timur). Depok: Universitas Indonesia; 2015.
34. Akhriani M, Fadhilah E, Kurniasari FN. Hubungan konsumsi minuman berpemanis dengan kejadian kegemukan pada remaja di SMP Negeri 1 Bandung. Indonesian Journal of Human Nutrition. 2016; 3 (1): 29–40.
35. Pries AM, Filteau S, Ferguson EL. Snack food and beverage consumption and young child nutrition in low- and middle-income countries: a systematic review. Matern Child Nutr. 2019; 15 (S4): 1–11.
36. Subdirectorates of Household Statistic, Central Bureau Statistic. Book 1: consumption and expenditure of population of Indonesia: based on the March 2017 Susenas. Jakarta: BPS-Statistics Indonesia; 2007.
37. Martin AA, Hamill LR, Davies S, Rogers PJ, Brunstrom JM. Energydense snacks can have the same expected satiation as sugar-containing beverages. Appetite. 2015; 95: 81–8.
38. Mattes RD. Dietary Compensation by humans for supplemental energy provided as ethanol or carbohydrate in fluids. Physiol Behav. 1996; 59 (1): 179–87.
39. DiMeglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes. 2000; 24 (6): 794–800.
40. Bellisle F, Rolland-Cachera MF. How sugar-containing drinks might increase adiposity in children. Lancet. 2001; 357 (9255): 490–1.
41. Must A, Barish EE, Bandini LG. Modifiable risk factors in relation to changes in BMI and fatness: what have we learned from prospective studies of school-aged children. Int J Obes. 2009; 33 (7): 705–15.
42. Marshall TA, Curtis AM, Cavanaugh JE, Warren JJ, Levy SM. Child and adolescent sugar-sweetened beverage intakes are longitudinally associated with higher body mass index z scores in birth cohort followed 17 years. J Acad Nutr Diet. 2019; 119 (3): 425–34.
43. Ma J, Fox CS, Jacques PF, Speliotes EK, Hoffmann U, Smith CE, et al. Sugar-sweetened beverage, diet soda, and fatty liver disease in the Framingham Heart Study cohorts. J Hepatol. 2015; 63 (2): 462–9.
44. Malik VS, Hu FB. Fructose and cardiometabolic health: what the evidence from sugar-sweetened beverages tells us. J Am Coll Cardiol. 2015; 66 (14): 1615–24.
45. Seferidi P, Millett C, Laverty AA. Sweetened beverage intake in association to energy and sugar consumption and cardiometabolic markers in children. Pediatr Obes. 2017; 13(4): 195–203.
46. de Boer EC, de Rooij SR, Olthof MR, Vrijkotte TGM. Sugar-sweetened beverages intake is associated with blood pressure and sympathetic nervous system activation in children. Clin Nutr ESPEN. 2018; 28: 232–5.
47. Malik AH, Akram Y, Shetty S, Malik SS, Yanchou Njike V. Impact of sugar-sweetened beverages on blood pressure. Am J Cardiol. 2014; 113 (9): 1574–80.
48. Palmer JR, Boggs DA, Krishnan S, Hu FB, Singer M, Rosenberg L. Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in African American women. Arch Intern Med. 2008; 168 (14): 1487– 92.
49. O’Neill KN, Fitzgerald AP, Kearney PM. Impact of population distribution shifts in sugar-sweetened beverage consumption on type II diabetes incidence in Ireland. Ann Epidemiol. 2020; 41: 1–6.
50. Chi DL, Scott JM. Added sugar and dental caries in children. Dent Clin North Am. 2019; 63 (1): 17–33.
51. Rebholz CM, Young BA, Katz R, Tucker KL, Carithers TC, Norwood AF, et al. Patterns of beverages consumed and risk of incident kidney disease. Clin J Am Soc Nephrol. 2019; 14 (1): 49–56.
52. Bomback AS, Derebail VK, Shoham DA, Anderson CA, Steffen LM, Rosamond WD, et al. Sugar-sweetened soda consumption, hyperuricemia, and kidney disease. Kidney Int. 2010; 77 (7): 609–16.
53. Yuzbashian E, Asghari G, Mirmiran P, Zadeh-Vakili A, Azizi F. Sugarsweetened beverage consumption and risk of incident chronic kidney disease: Tehran lipid and glucose study. Nephrology. 2016; 21 (7): 608–16.
54. Gibson S, Boyd A. Associations between added sugars and micronutrient intakes and status: further analysis of data from the National Diet and Nutrition Survey of Young People aged 4 to 18 years. Br J Nutr. 2009; 101 (1): 100–7.
55. Louzada ML da C, Martins APB, Canella DS, Baraldi LG, Levy RB, Claro RM, et al. Impact of ultra-processed foods on micronutrient content in the Brazilian diet. Rev Saude Publica. 2015; 49.
56. Maunder EMW, Nel JH, Steyn NP, Kruger HS, Labadarios D. Added sugar, macro- and micronutrient intakes and anthropometry of children in a developing world context. PLoS One. 2015; 10 (11): 1–24.
57. Fulgoni VL, Gaine PC, Scott MO, Ricciuto L, DiFrancesco L. Association of added sugars intake with micronutrient adequacy in U.S. Children and Adolescents: NHANES 2009–2014. Curr Dev Nutr. 2019; 6: 1–11.
58. Chazelas E, Srour B, Desmetz E, Kesse-Guyot E, Julia C, Deschamps V, et al. Sugary drink consumption and risk of cancer: results from NutriNet-Santé prospective cohort. BMJ. 2019; 366.
59. Mossavar-Rahmani Y, Kamensky V, Manson JAE, Silver B, Rapp SR, Haring B, et al. Artificially sweetened beverages and stroke, coronary heart disease, and all-cause mortality in the women’s health initiative. Stroke. 2019; 50 (3): 555–62.
60. Prather AA, Leung CW, Adler NE, Ritchie L, Laraia B, Epel ES. Short and sweet: associations between self-reported sleep duration and sugar-sweetened beverage consumption among adults in the United States. Sleep Health. 2016; 2 (4): 272–6.
61. Geng M, Jiang L, Wu X, Ding P, Liu W, Liu M, et al. Sugar-sweetened beverages consumption are associated with behavioral problems among preschoolers: a population based cross-sectional study in China. J Affect Disord. 2020; 265: 519–25.
62. Malik VS, Li Y, Pan A, De Koning L, Schernhammer E, Willett WC, et al. Long-term consumption of sugar-sweetened and artificially sweetened beverages and risk of mortality in US adults. Circulation. 2019; 139 (18): 2113–25.
63. World Bank Open Data. data.worldbank.org; 2020.
64. Ministry of Health Republic of Indonesia. National basic health research (Riskesdas) 2013. Jakarta; Ministry of Helath Republic of Indonesia; 2013.
65. Ministry of Health Republic of Indonesia. National basic health research (Riskesdas) 2007. Jakarta: Ministry of Health of Republic of Republic Indonesia; 2007.
Recommended Citation
Sartika RD , Atmarita A , Duki M ,
et al.
Consumption of Sugar-Sweetened Beverages and Its Potential Health Implications in Indonesia.
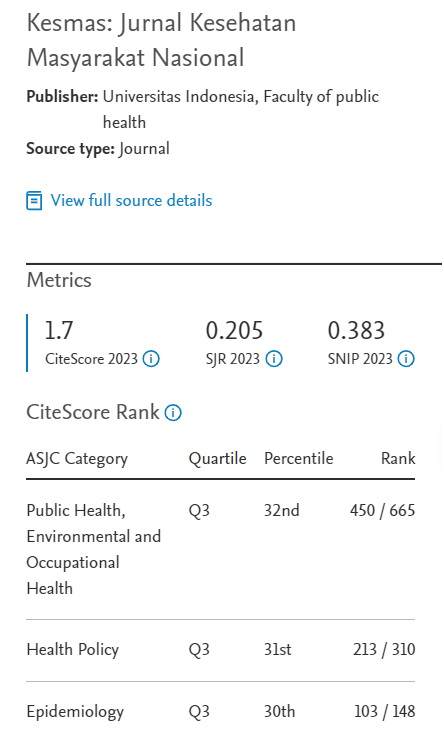
Kesmas.
2022;
17(1):
1-9
DOI: 10.21109/kesmas.v17i1.5532
Available at:
https://scholarhub.ui.ac.id/kesmas/vol17/iss1/1
Included in
Biostatistics Commons, Environmental Public Health Commons, Epidemiology Commons, Health Policy Commons, Health Services Research Commons, Nutrition Commons, Occupational Health and Industrial Hygiene Commons, Public Health Education and Promotion Commons, Women's Health Commons