Abstract
Socio-cultural concerns often restrict women's sexual rights and well-being living with HIV (WLHIV) in developing countries. These convergent parallel mixed methods study combined quantitative and qualitative approaches to explore factors influencing WLHIV sexual quality of life in Banten Province, Indonesia. A 2017 cross-sectional survey of 207 reproductive-aged WLHIV was analyzed using univariate and multivariate logistic regression statistics. Furthermore, in-depth interviews with a sub-sample of survey participants (n = 30) were thematically analyzed. Most of the women (60%) involved reported loss of sexual pleasure and depressed sexual life. Meanwhile, 48% affirmed low sexual quality of life which was associated with unemployment (aOR = 2.90, and 95%CI =1.51–5.58), limited sexual activities (aOR = 2.89, and 95%CI = 1.20–6.93), living with extended family (aOR = 2.68, and 95%CI = 1.27–5.65), and experiencing intimate partner violence (aOR = 2.28, and 95%CI = 1.03–5.03). The respondents described unsatisfactory sexual life in a belief that having sex is a wife's duty and choosing not to talk about sexual issues or refuse sexual invitation in fear of triggering intimate partner violence. Inter-related personal, social, cultural, and religious factors affected the sufferers’ sexual life.
References
1. Joint United Nations Programme on HIV and AIDS. Global HIV & AIDS statistics - 2020 fact sheet. Geneva: UNAIDS; 2020.
2. Kementerian Kesehatan Republik Indonesia. Profil kesehatan Indonesia tahun 2019. Jakarta: Kementerian Kesehatan Republik Indonesia; 2020.
3. Kementerian Kesehatan Republik Indonesia. Laporan perkembangan HIV-AIDS triwulan I tahun 2020. Jakarta: Direktorat Jenderal Pencegahan dan Pengendalian Penyakit, Kementerian Kesehatan Republik Indonesia; 2020.
4. Khosla R, Van Belle N, Temmerman M. Advancing the sexual and reproductive health and human rights of women living with HIV: a review of UN, regional and national human rights norms and standards. Journal of the International AIDS Society. 2015; 18 (Suppl 5): 20280.
5. United Nations Population Fund. Sexual and reproductive health. Washington DC.: UNFPA; 2021.
6. World Health Organization. Consolidate guideline on sexual and reproductive health and rights of women living with HIV. Geneva: World Health Organization; 2017.
7. Adekanle DA, Olowookere SA, Adewole AD, Adeleke NA, AbioyeKuteyi EA, Ijadunola MY. Sexual experiences of married HIV positive women in Osogbo, Southwest Nigeria: role of inappropriate status disclosure. BMC Women's Health. 2015; 15: 6.
8. Maeri I, El Ayadi A, Getahun M, Charlebois E, Akatukwasa C, Tumwebaze D, et al. "How can I tell?" Consequences of HIV status disclosure among couples in Eastern African communities in the context of an ongoing HIV "test-and-treat" trial. AIDS care. 2016; 28 Suppl 3: 59-66.
9. Closson EF, Mimiaga MJ, Sherman SG, Tangmunkongvorakul A, Friedman RK, Limbada M, et al. Intimacy versus isolation: a qualitative study of sexual practices among sexually active HIV-infected patients in HIV care in Brazil, Thailand, and Zambia. PloS one. 2015; 10 (3): e0120957.
10. Kaida A, Carter A, de Pokomandy A, Patterson S, Proulx-Boucher K, Nohpal A, et al. Sexual inactivity and sexual satisfaction among women living with HIV in Canada in the context of growing social, legal and public health surveillance. Journal of the International AIDS Society. 2015; 18 (Suppl 5): 20284.
11. World Health Organization. Sexual health, human rights and the law. Geneva: World Health Organization; 2015.
12. Chakraborty H, Patted S, Gan A, Islam F, Revankar A. Determinants of Intimate Partner Violence Among HIV-Positive and HIV-Negative Women in India. J Interpers Violence. 2016; 31 (3): 515-30.
13. Chin YM. Does HIV increase the risk of spousal violence in subSaharan Africa?. Journal of health economics. 2013; 32 (5): 997-1006.
14. Okareh OT, Akpa OM, Okunlola JO, Okoror TA. Management of conflicts arising from disclosure of HIV status among married women in southwest Nigeria. Health Care for Women International. 2015; 36 (2): 149-60.
15. Juliastuti D, Dean J, Fitzgerald L. Sexual and reproductive health of women living with HIV in Muslim-majority countries: a systematic mixed studies review. BMC International Health and Human Rights. 2020; 20 (1): 5.
16. Creswell JW. Research design: qualitative, quantitative, and mixedmethods approaches. Sage Publications; 2013.
17. Kaur M. Application of mixed method approach in public health re - search. Indian Journal of Community Medicine: Official Publication of Indian Association of Preventive & Social Medicine. 2016; 41 (2): 93- 7.
18. Shorten A, Smith J. Mixed methods research: expanding the evidence base. Evidence Based Nursing. 2017; 20 (3): 74-5.
19. Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Sage Publications. 2017.
20. Dinas Kesehatan Provinsi Banten. Profil kesehatan Provinsi Banten 2015 Serang, Banten; 2016.
21. Reaves CC. Quantitative research for the behavioral sciences. New York: John Wiley & Sons, Inc.; 1992.
22. Statistics Indonesia, National Population and Family Planning Board, Kementrian Kesehatan Republik Indonesia, ICF International. Indonesia demographic and health survey 2012. Jakarta, Indonesia: BPS, BKKBN, Kemenkes, ICF International; 2013.
23. Symonds T, Boolell M, Quirk F. Development of a questionnaire on sexual quality of life in women. Journal of Sex & Marital Therapy. 2005; 31 (5): 385-97.
24. Pallant J. SPoS survival manual: a step by step guide to data analysis using IBM SPSS. 6th ed. London, UK: McGraw-Hill Education; 2016.
25. Ranganathan P, Pramesh CS, Aggarwal R. Common pitfalls in statistical analysis: logistic regression. Perspectives in Clinical Research. 2017; 8 (3): 148-51.
26. Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health. 2018; 6: 149.
27. Brown KM, Elliott SJ, Leatherdale ST, Robertson-Wilson J. Searching for rigour in the reporting of mixed methods population health research: a methodological review. Health Education Research. 2015; 30 (6): 811-39.
28. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006; 3 (2): 77-101.
29. Padgett D. Qualitative and mixed methods in public health. Thousand Oaks, California: Sage Publications, Inc; 2012.
30. Curry LA, Nembhard IM, Bradley EH. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009; 119 (10): 1442-52.
31. Guetterman TC, Fetters MD, Creswell JW. Integrating quantitative and qualitative results in health science mixed methods research through joint displays. Annals of Family Medicine. 2015; 13 (6): 554- 61.
32. El Fane M, Bensghir R, Sbai S, Chakib A, Kadiri N, Ayouch A, et al. Quality of sexual life for people living with HIV (PLWHA). Sexologies. 2011; 20 (3): 158-62.
33. Utomo ID, McDonald P. Adolescent Reproductive Health in Indonesia: Contested Values and Policy Inaction. Studies in family planning. 2009; 40 (2): 133-46.
34. Bennett LR. Zina and the enigma of sex education for Indonesian Muslim youth. Sex Education. 2007; 7 (4): 371-86.
35. Amin A. Addressing gender inequalities to improve the sexual and reproductive health and wellbeing of women living with HIV. Journal of the International AIDS Society. 2015; 18 (6S5): 20302.
36. Bennett LR, Davies SG. Sex and sexualities in contemporary Indonesia: sexual politics, health, diversity and representations. Routledge; 2014.
37. Aisyah S, Parker L. Problematic conjugations: women’s agency, marriage and domestic violence in Indonesia. Asian Studies Review. 2014; 38 (2): 205-23.
38. Jacubowski N. Marriage is not a safe place: heterosexual marriage and HIV-related vulnerability in Indonesia. Culture, Health and Sexuality. 2008; 10 (1): 87-97.
39. Puradiredja DI, Coast E, Sear R. Why do female sex workers in Indonesia not use condoms?: a mixed methods study of the heterogeneous contexts of condom use. European Population Conference; Barcelona, Spain: LSE Research Online; 2008.
40. Shahhosseini Z, Gardeshi ZH, Pourasghar M, Salehi F. A review of affecting factors on sexual satisfaction in women. Materia Socio-Medica. 2014; 26 (6): 378-81.
41. United Nations Development Programme, WAP+, APN+, Unzip the Lips. Discussion paper: linkages between violence against women and HIV in Asia and the Pacific. Bangkok: UNDP; 2013.
42. Anwar N, Khan SI. Sexual life after HIV infection: an exploratory study among HIV positive adult males and females in Dhaka, Bangladesh. International Journal of Interdisciplinary Social Sciences. 2010; 5( 2): 589-602.
43. Richter L, Rotheram-Borus MJ, Van Heerden A, Stein A, Tomlinson M, Harwood JM, et al. Pregnant women living with HIV (WLH) supported at clinics by peer WLH: a cluster randomized controlled trial. AIDS and Behavior. 2014; 18 (4): 706-15.
44. Robinson JL, Narasimhan M, Amin A, Morse S, Beres LK, Yeh PT, et al. Interventions to address unequal gender and power relations and improve self-efficacy and empowerment for sexual and reproductive health decision-making for women living with HIV: a systematic review. PloS one. 2017; 12 (8): e0180699-e.
Recommended Citation
Juliastuti D , Dean J , Afiyanti Y ,
et al.
Inter-related Factors Influencing Sexual Quality of Life among Women Living with HIV in Banten Province, Indonesia: A Mixed Methods Study.
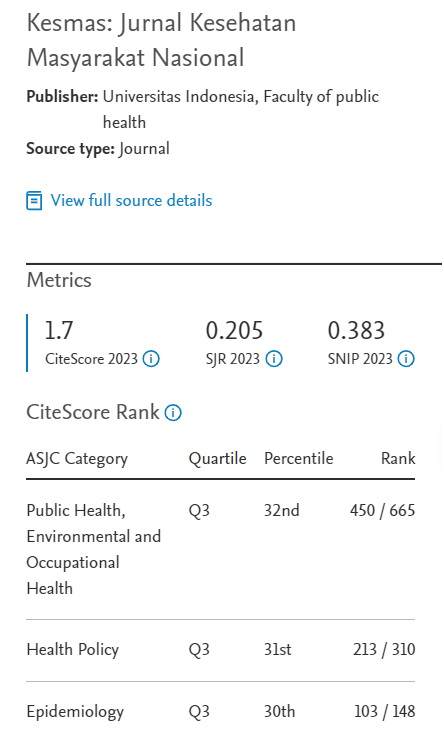
Kesmas.
2021;
16(2):
120-130
DOI: 10.21109/kesmas.v16i2.4862
Available at:
https://scholarhub.ui.ac.id/kesmas/vol16/iss2/9
Included in
Biostatistics Commons, Environmental Public Health Commons, Epidemiology Commons, Health Policy Commons, Health Services Research Commons, Nutrition Commons, Occupational Health and Industrial Hygiene Commons, Public Health Education and Promotion Commons, Women's Health Commons