Abstract
The case of COVID-19 in Indonesia continues to increase, transmitted directly and indirectly. Hygiene and sanitation approaches are needed for prevention. The purpose of this review is to review how the transmission COVID-19, the challenges of Indonesia, and the policy of COVID-19 prevention with hygiene and sanitation approaches. The results show Indonesia's challenges namely urban area density, air pollution, and smokers, low hand washing habits, low ac- cess to clean water and drinking water, open defecation behavior, limited personal protective equipment. COVID-19 control policy with the hygiene sanitation approach is carried out with 4 factors namely personal protect equipment, health education, personal hygiene, and sanitation.
References
1. Oon-Tek Ng, Kalisvar Marimuthu, Po-Ying Chia, Vanessa Koh P, Calvin JC, Liang DW, et al. SARS-CoV-2 infection among travelers returning from Wuhan, China. The New England Jurnal of Medicine. 2020; 382: 1476-8. 2. Zhang D, Wang W, Xingwang, Yang B et al. A novel coronavirus from patients with pneumonia in China, 2019. The New England Jurnal of Medicine. 2020; 382 (8): 727–33. 3. World Health Organization. WHO director - general’s opening remarks at the media briefing on COVID-19 - 11 March 2020. Geneva; 2020. 4. Callaway BE, Cyranoski D, Mallapaty S, Stoye E, Tollefson J. Coronavirus by the numbers. Nature. 2020; 579 (7800): 482–3. 5. World Health Organization. Coronavirus disease (COVID-2019) situation reports. Geneva; 2020. 6. Badan Pusat Statistik. Jumlah kunjungan wisatawan mancanegara. Indonesia; 2019. 7. Badan Nasional Penanggulangan Bencana. Report COVID-19 in Indonesia. 2020. 8. Liu YC, Liao CH, Chang, Chou CC, Lin YR. A locally transmitted case of SARS-CoV-2 infection in Taiwan. The New England Jurnal of Medicine. 2020; 382 (11): 1070-2. 9. Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of corona-viruses on inanimate surfaces and their inactivation with biocidal agents. Journal of Hospital Infection. 2020; 104 (3): 246–51. 10. Ghinai I, Mcpherson TD, Hunter JC, Kirking HL, Christiansen D, Joshi K, et al. Articles first known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet. 2020; 395: 1137–44. 11. Qun Li, Xuhua Guan, Peng Wu, Xiaoye Wang, Lei Zhou, Yeqing Tong, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. The New England Jurnal of Medicine. 2020; 382: 1199–207. 12. Deng S, Peng H. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. Journal of Clinical Medicine. 2020; 9 (2): 575. 13. World Health Organization. COVID-19. Geneva; 2020. 14. Colavita F, Lapa D, Carletti F, Lalle E, Bordi L, Marsella P, et al. SARS-CoV-2 isolation from ocular secretions of a patient with COVID-19 in Italy with prolonged viral RNA detection. Annals of Internal Medicine. 2020; M20-1176. 15. Adhikari SP, Meng S, Wu Y, Mao Y, Ye R, Wang Q, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease ( COVID-19 ) during the early outbreak period: a scoping review. Infectious Disease of Poverty. 2020; 9 (29): 1–12. 16. Kementerian Kesehatan Republik Indonesia. Riset kesehatan dasar 2018. Jakarta; 2018. 17. Chen C, Guiju G, Yanli Xu, Lin P, Qi W, Liming W et al. SARS-CoV-2–positive sputum and feces after conversion of pharyngeal samples in patients with COVID-19. Annals of Internal Medicine. 2020; 172 (12): 832-4. 18. Mallapaty S. How sewage could reveal true scale of coronavirus outbreak. Nature. 2020; 580 (7802): 176-7. 19. World Health Organization. Water sanitation hygiene; 2012. 20. Joint World Health Organization/United Nations Children’s Fund Press Release. Progress on household drinking water, sanitation and hygiene 2000-2017: special focus on inequalities. New York; 2019. 21. Sub Direktorat Statistik Rumah Tangga. Indonesia - survei sosial ekonomi nasional 2017 maret (KOR). Jakarta: Badan Pusat Statistik; 2018: pp. 1–230. 22. Pan Zhai, Yanbing Ding, Xia Wu, Junke Long, Yanjun Zhong, Yimng Li. The epidemiology, diagnosis and treatment of COVID-19. International Journal of Antimicrobial Agents. 2020; 55 (5): 105955. 23. Chih-Cheng L, Tzu-Ping S, Wen-Chien K, Hung-Jen T, Po-Ren H. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. International Journal of Antimicrobial Agents. 2020; 55 (3): 105924. 24. World Health Organization. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations; 2020. 25. Chan JFW, Yuan S, Kok KH, To KKW, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020; 395 (10223): 514–23. 26. Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV- 2) from a symptomatic patient. JAMA. 2020; 323 (16): 1610-2. 27. Wu Y, Chen C, Chan Y. The outbreak of COVID-19: an overview. Journal of the Chinese Medical Association. 2020; 83 (3): 217–20. 28. Doremalen Nv, Bushmaker T, Morris H, Holbrook M G, Gamble A, Williamson B N, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. The New England Journal of Medicine. 2020; 382:1564-7. 29. Bai Y, Yao L, Wei T, Tian F, Jin D Y, Chen L, et al. Presumed asymptomatic carrier transmission of COVID 19. The New England Journal of Medicine. 2020; 323 (14): 1406-7. 30. Lirong Z, Feng R, Mingxing H, Lijun L, Huitao H, Zhongsi H, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. The New England Journal of Medicine. 2020; 382: 1177-9. 31. Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-nCOV infection from an asymptomatic contact in Germany. The New England Journal of Medicine. 2020; 382: 970–1. 32. Jordan H. COVID-19: fecal-oral transmission?. Nature Review Gastroenterology & Hepatology. 2020; 17 (5): 259. 33. Lodder W, Husman AMdR. SARS-CoV-2 in wastewater: potential health risk, but also data source. Lancet Gastroenterology Hepatology. 2020; 5 (6): 533–4. 34. Chih-Cheng L, Yen Hung L, Cheng-Yi W, Ya-Hui W, Shun-Chung H, Muh-Yen Y, et al. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): facts and myths. Journal of Microbio logy, Immunology and Infection. 2020; 53 (3): 404-12. 35. Wells CR, Sah P, Moghadas SM, Pandey A, Shoukat A, Wang Y, et al. Impact of international travel and border control measures on the global spread of the novel 2019 coronavirus outbreak. PNAS-Proceedings of the National Academy of Sciences of the United States of America. 2020; 117 (13): 7504–9. 36. Lewnard JA, Lo NC. Scientific and ethical basis for social-distancing interventions against COVID-19. The Lancet Infectious Diseases. 2020; 20 (6): 631–3. 37. Prem K, Liu Y, Russell TW, Kucharski AJ, Eggo RM, Davies N, et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modeling study. The Lancet Public Health. 2020; 5 (5): 261-70. 38. Badan Pusat Statistik. Survei Sosial Ekonomi Nasional. Jakarta; 2017. 39. Atkinson J, Chartier Y, Silva CLP, Jensen P, Yuguo L, and Seto WH. Natural ventilation for infection control in health-care settings - NCBI bookshelf. Geneva: World Health; 2009. 40. Gao X, Wei J, Lei H, Xu P, Cowling BJ, Li Y. Building ventilation as an effective disease intervention strategy in a dense indoor contact network in an ideal city. PLoS One. 2016; 11 (9): e0162481. 41. Qian H, Zheng X. Ventilation control for airborne transmission of human exhaled bio-aerosols in buildings. Journal of Thoracic Disease. 2018; 10 (Suppl 19): S2295–304. 42. Greenstone M, Fan Q. Indonesia’s worsening air quality and its impact on life expectancy. Air Quality Life Index; 2019. 43. Conticini E, Frediani B, Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy?. Environmental Pollution. June 2020; 261: 114465. 44. Sun Z, Zhu D. Exposure to outdoor air pollution and its human-related health outcomes: an evidence gap map. BMJ Open 2019; 9: e031312. 45. Sweileh WM, Al-Jabi SW, Zyoud SH, Sawalha AF. Outdoor air pollution and respiratory health: a bibliometric analysis of publications in peer-reviewed journals (1900 - 2017). Multidisciplinary Respiratory Medicine. 2018; 13: 15 (1-12). 46. Ghorani-Azam A, Riahi-Zanjani B, Balali-Mood M. Effects of air pollution on human health and practical measures for prevention in Iran. Journal of Research in Medical Sciences. 2016; 21: 65. 47. World Health Organization. Burden of disease from the joint effects of household and ambient air pollution for 2016: summary of results; 2018. 48. Kementerian Kesehatan Republik Indonesia. Diseases report; 2018. 49. Mark Drajem, Lorraine Woellert. Clove cigarettes may prompt U.S., Indonesia dispute. Southeast Asia Tobacco Control Alliance. 2018; pp. 1–144. 50. Infodatin. Situasi umum konsumsi tembakau di Indonesia. Jakarta: Kementerian Kesehatan Republik Indonesia; 2019. 51. World Health Organization. Tobacco free initiative: tobacco and waterpipe use increases the risk of suffering from COVID-19; 2020. 52. Terzikhan N, Verhamme KMC, Hofman A, Stricker BH, Brusselle GG, Lahousse L. Prevalence and incidence of COPD in smokers and non-smokers: the Rotterdam study. European Journal of Epidemiology. 2016; 31 (8): 785–92. 53. Vardavas C, Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tobacco Induced Diseases. 2020; 18: 20. 54. World Health Organization. Improve hand hygiene practices widely to help prevent the transmission of the COVID-19; 2020. 55. Hirai M, Graham JP, Mattson KD, Kelsey A, Mukherji S, Cronin AA. Exploring determinants of handwashing with soap in Indonesia: a quantitative analysis. International Journal of Environmental Research and Public Health. 2016; 13 (9): 868. 56. Patunru AA. Access to safe drinking water and sanitation in Indonesia. Asia & Pacific Policy Studies. 2015; 2 (2): 234–44. 57. Kementerian Lingkungan Hidup & Kehutanan Republik Indonesia. Laporan Kinerja Kementerian Lingkungan Hidup dan Kehutanan Tahun 2017; 2018. 58. Tang A, Tong Z-d, Wang H-l, Dai Y-x, Li K-f, Liu J-n, et al. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerging Infectious Disease. 2020; 26 (6). 59. World Bank Group. Water supply and sanitation in Indonesia turning finance into service for the future. Washington; 2015: pp. 1–88. 60. World Bank. September 2013. World Bank: Washington; 2013. 61. World Health Organization. Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19); 2020. 62. Yi Y, Lagniton PNP, Ye S, Li E, Xu R. COVID-19: what has been learned and to be learned about the novel coronavirus disease. International Journal of Biological Sciences. 2020; 16 (10): 1753–66. 63. Huang S. COVID-19: why we should all wear mask— there is new scientific rationale. Medium. 2020; 64. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323 (11): 1061–9. 65. Gugus Tugas Percepatan Penanganan COVID-19. Pedoman penangan cepat medis dan kesehatan masyarakat COVID-19 di Indonesia. Jakarta; Maret 2020: pp.1-38. 66. Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian Journal of Psychiatry. 2020; 51: 102083. 67. Yuen KS, Ye ZW, Fung SY, Chan CP, Jin DY. SARS-CoV-2 and COVID-19: the most important research questions. Cell & Bioscience. 2020; 10 (40). 68. Gormley M, Aspray TJ, Kelly DA. COVID-19: mitigating transmission via wastewater plumbing systems. The Lancet Global Health. 2020; 8 (5): e643. 69. Cameron L, Olivia S, Shah M. Scaling up sanitation: evidence from an RCT in Indonesia. Journal of Development Economics. 2019; 138: 1– 16. 70. Venkataramanan V, Crocker J, Karon A, Bartram J. Community-led total sanitation: a mixed-methods systematic review of evidence and its quality. Environmental Health Perspectives. 2018; 126 (2): 026001. 71. Zuin V, Delaire C, Peletz R, Cock-Esteb A, Khush R, Albert J. Policy diffusion in the rural sanitation sector: lessons from community-led total sanitation (CLTS). World Development. 2019; 124: 104643.
Recommended Citation
Purnama SG , Susanna D .
Hygiene and Sanitation Challenge for COVID-19 Prevention in Indonesia.
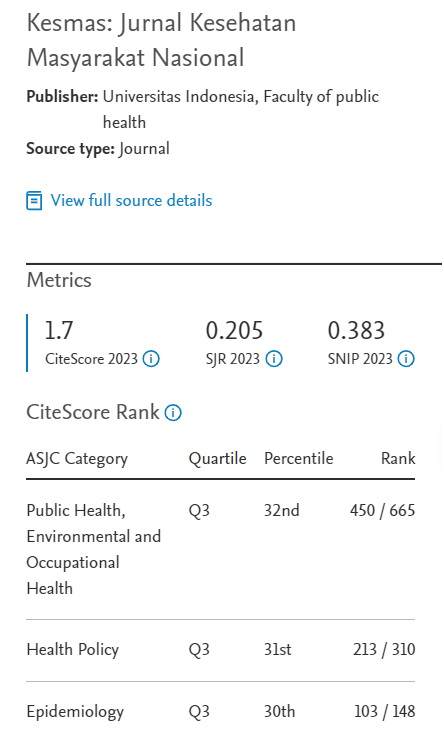
Kesmas.
2020;
15(5):
6-13
DOI: 10.21109/kesmas.v15i2.3932
Available at:
https://scholarhub.ui.ac.id/kesmas/vol15/iss5/2