Abstract
Infectious diseases are one of the top ten causes of death in the world. Antibiotic therapy is administered for infectious diseases, but if bacteria are exposed to antibiotics continuously, then the bacteria are able to adapt to the medication, thereby resulting in antibiotic resistance. This condition results in an increase in mortality, long hospitalization period, and increased cost of antibiotic therapy and health services. Adherence to using antibiotics may be influenced by knowledge and beliefs about them. This study aimed to understand correlation between knowledge and belief with adherence to antibiotic use at a private hospital in Sidoarjo. This cross-sectional study, the data collected in three months period, was conducted with a questionnaire for assessment knowledge and belief. A pill count method was applied for assessment adherence to using antibiotics prescribed by doctors. The study results show that knowledge of the respondents was adequate for 76 people (69.7%), belief was adequate for 74 people (67.9%), and adherence to antibiotic use for 79 people (72%). Regression analysis showed that the variable that significantly influenced the adherence of patients in using antibiotics was perceived threat (p-value = 0,029). Sex, age, education, income, occupation, and marital status have no contribution to antibiotic knowledge, belief, and adherence.
References
1. Etebu E, Arikekpar I. Antibiotics: classification and mechanisms of action with emphasis on molecular perspectives. International Journal of Applied Microbiology and Biotechnology Research. 2016; 4: 90–101.
2. World Health Organization. Antimicrobial resistance: global report on surveillance 2014. Geneva, Switzerland: WHO Press; 2014.
3. World Health Organization. Antimicrobial resistance: global action plan on antimicrobial resistance. Geneva, Switzerland: WHO Press; 2015.
4. Kourkouta L, Kotsiftopoulos C, Papageorgiou M, Iliad, Monios A. The rational use of antibiotics medicine. Journal of Healthcare Communication. 2017; 2: 36.
5. Karen G, Barbara K, Rimer KV. Health behavior and health education: theory, research, and practice, fifth edition. San Fransisco: Jossey-Bass (A Wiley Brand); 2015. p. 47–50.
6. Insany AN, Destiani DP, Sani A, Sabdaningtyas L, Pradipta IS. Association between perceived value and self-medication with antibiotics: an observational study based on health belief model theory. Jurnal Farmasi Klinik Indonesia. 2015; 4 (2): 77–86.
7. Chalvy W, Lily RG. Pengaruh penyuluhan penggunaan antibiotika terhadap tingkat pengetahuan masyarakat di Kota Manado. Pharmacon. 2013; 2 (3): 24-8.
8. Kelly GR, Mamon JA, Scott JE. Utility of the health belief model in examining medication compliance among psychiatric outpatients among psychiatric outpatients. Social Science & Medicine. 1987; 25 (11): 1205-11.
9. Ventola CL. The antibiotic resistance crisis part 1: causes and threats. Physical Therapy. 2015; 40 (4): 277–83.
10 Shamna M, Dilip C, Ajmal M, Linu Mohan P, Shinu C, Jafer CP, et al. A prospective study on adverse drug reactions of antibiotics in a tertiary care hospital. Saudi Pharmaceutical Journal. 2014; 22 (4): 303–8.
11. Allen K, Farah CS, Brame JL Tavoc T, Stein M, Curran AE MR, et al. Antibiotic guidelines 2015-2016: treatment recommendations for adult inpatients. Johns Hopkins Medicine; 2016.
12. Kalogianni A. Factors affect in patient adherence to medication regimen. Health Science Journal. 2011; 5 (3): 157–8.
13. Yosmar R, Fitria A, Yuliandra Y, Arifin H. Evaluation of parents’ adherence in giving antibiotics on respiratory tract infections (RTI) and factors associated with adherence. Research Journal of Pharmaceutical, Biological and Chemical Sciences. 2016; 7 (1): 1662– 5.
14. Yaheya M, Ismail M. Drug-food interactions and role of pharmacist. Asian Journal Pharmaceutical Clinical Research. 2009; 2 (4): 1–10.
15. Awad AI, Aboud EA. Knowledge, attitude and practice towards anti - biotic use among the public in Kuwait. PLoS One. 2015; 10 (2): e0117910.
16. Chan YH, Fan MM, Fok CM, Lok ZL, Ni M, Sin CF, et al. Antibiotics nonadherence and knowledge in a community with the world’s leading prevalence of antibiotics resistance: implications for public health intervention. American Journal Infection Control. 2012; 40 (2): 113–7.
17. Muñoz EB, Dorado MF, Guerrero JE, Martínez FM. The effect of an educational intervention to improve patient antibiotic adherence during dispensing in a community pharmacy. Aten Primaria. 2014; 46 (7): 367–75.
18. Al-Shibani N, Hamed A, Labban N, Al-Kattan R, Al-Otaibi H, Alfadda S. Knowledge, attitude and practice of antibiotic use and misuse among adults in Riyadh, Saudi Arabia. Saudi Medical Journal. 2017; 38 (10): 1038–44.
19. Roope LSJ, Tonkin-crine S, Butler CC, Crook D, Peto T, Peters M, et al. Reducing demand for antibiotic prescriptions: evidence from an online survey of the general public on the interaction between preferences, beliefs and information, United Kingdom, 2015. Eurosurveillance. 2018; 23 (25).
20. Waaseth M, Adan A, Røen IL, Eriksen K, Stanojevic T, Halvorsen KH, et al. Knowledge of antibiotics and antibiotic resistance among Norwegian pharmacy customers - a cross-sectional study. BMC Public Health. 2019; 19 (1): 66.
21. Jose J, Jimmy B, Mohammed Saif AlSabahi AG, Al Sabei GA. A study assessing public knowledge, belief and behavior of antibiotic use in an Omani population. Oman Medical Journal. 2013; 28 (5): 324–30.
22. Kandrotaite K, Smigelskas K, Janusauskiene D, Jievaltas M, Maciulaitis R, Briedis V. Development of a short questionnaire to identify the risk of nonadherence to antibiotic treatment. Current Medical Research and Opinion. 2013; 29 (11): 1555–63.
23. Shehadeh M, Suaifan G, Darwish RM, Wazaify M, Zaru L, Alja’fari S. Knowledge, attitudes and behavior regarding antibiotics use and misuse among adults in the community of Jordan. A pilot study. Saudi Pharmaceutical Journal. 2012; 20 (2): 125–33.
4. Eglė P, Vincentas V, Asta M, Mačiulis V, Kęstutis P, Stankevičius E. Public knowledge, beliefs and behavior on antibiotic use and self-medi - cation in Lithuania. International Journal of Environmental Research and Public Health. 2015; 12 (6): 7002-16.
25. Widayati A, Suryawati S, de Crespigny C, Hiller JE. Knowledge and beliefs about antibiotics among people in Yogyakarta City Indonesia: a cross sectional population-based survey. Antimicrobial and Infection Control. 2012; 1 (1): 38.
26. Kouhpayeh A, Jeihooni AK, Kashfi SH, Bahmandoost M. Effect of an educational intervention based on the model of health beliefs in selfmedication of Iranian mothers. Investigación y Educación en Enfermería. 2017; 35 (1): 59–68.
27. Bakhit M, Del Mar C, Gibson E, et al. Exploring patients’ understanding of antibiotic resistance and how this may influence attitudes towards antibiotic use for acute respiratory infections: a qualitative study in Australian general practice. BMJ Open. 2019; 9: e026735.
Recommended Citation
Wattiheluw MH , Herawati F , Setiasih S ,
et al.
Correlation of Knowledge and Beliefs to Adherence with Antibiotic Use in Adult Patients at a Private Hospital in Sidoarjo.
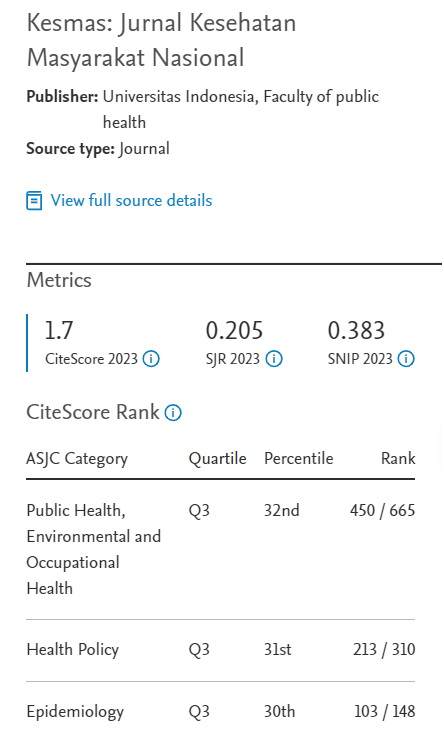
Kesmas.
2020;
15(2):
99-104
DOI: 10.21109/kesmas.v15i2.2409
Available at:
https://scholarhub.ui.ac.id/kesmas/vol15/iss2/8
Included in
Biostatistics Commons, Environmental Public Health Commons, Epidemiology Commons, Health Policy Commons, Health Services Research Commons, Nutrition Commons, Occupational Health and Industrial Hygiene Commons, Public Health Education and Promotion Commons, Women's Health Commons