Abstract
The World Health Organization estimated that chronic obstructive pulmonary disease (COPD) will be the highest non-communicable disease worldwide by2030, and pesticide exposure is one of major risk factors. This study aimed to determine effect of pesticide exposure on lung dysfunction among paddyfarmers. A case-control study was performed on April - May 2016 in Purworejo. The case group comprised 66 farmers suffering from lung dysfunction during2015 based on medical records, while the control group comprised 59 neighboring farmers showing normal lung function. Both case and control groups weretested using a spirometer and COPD assessment test (CAT) questionnaire. Logistic regression analysis of pesticide quantity (OR = 0.75; 95% CI = 0.317 -1.754) and duration of spraying (OR = 1.11; 95% CI = 0.430 - 2.891) adjusted for confounders showed no clear associations. Pesticide remained a potentialhealth risk for lung dysfunction due to farming duration (OR = 5.61; 95% CI = 1.124 - 27.990) adjusted by age, personal protective equipment, records of lungdisease, smoking habit, dust exposure, and indoor air pollution. The farming duration was revealed to be a risk factor, but no clear association was found between quantity and duration of spraying to lung dysfunction.
References
1. Perret JL, Walters EH, Abramson MJ, Mcdonald CF, Dharmage SC. The independent and combined effects of lifetime smoke exposures and asthma as they relate to COPD. Expert Review of Respiratory Medicine. 2014; 8 (4): 503-14.
2. Rinsky JL. The role of occupational exposure to animal production in chronic obstructive pulmonary disease among farmers in Iowa and North Carolina. University of North Carolina; 2015.
3. Buralli RJ, Ribeiro H, Mauad T, Amato-Lourenço LF, Salge JM, DiazQuijano FA, et al. Respiratory condition of family farmers exposed to pesticides in the State of Rio de Janeiro, Brazil. International Journal of Environmental Research and Public Health. 2018; 15(6).
4. Nurcandra F, Mahkota R, Shivalli S. Effect of personal protective equipment during pesticide application to neurological symptoms in farmers in Purworejo District, Indonesia. Kesmas: National Public Health Journal. 2018; 12(4): 165–71.
5. Ye M, Beach J, Martin JW, Senthilselvan A. Occupational pesticide exposures and respiratory health. International Journal of Environmental Research and Public Health. 2013; 10 (12): 6442–71.
6. de Jong K, Boezen H, Kromhout H, Vermeulen R, Postma D, Vonk J. Pesticides and other occupational exposures are associated with airway obstruction: the LifeLines cohort study. Journal of Occupational and Environmental Medicine. 2014; 71 (2): 88–96.
7. Abu Sham’a F, Skogstad M, Nijem K, Bjertness E, Kristensen P. Lung function and respiratory symptoms in male Palestinian farmers. Archives of Environmental & Occupational Health. 2010; 65 (4): 191–200.
8. Damalas CA, Eleftherohorinos IG. Pesticide exposure, safety issues, and risk assessment indicators. International Journal of Environmental Research and Public Health. 2011; 8 (5): 1402–19.
9. Fareed M, Pathak MK, Bihari V, Kamal R, Srivastava AK, Kesavachandran CN. Adverse respiratory health and hematological alterations among agricultural workers occupationally exposed to organophosphate pesticides: a cross-sectional study in North India. PLoS One. 2013; 8 (7): e69755.
10. Sapbamrer R, Nata S. Health symptoms related to pesticide exposure and agricultural tasks among rice farmers from Northern Thailand. Environmental Health and Preventive Medicine. 2014; 19 (1): 12–20.
11. Zhu X, Gao P, Gu Y, Xiao P, Liu M, Chen J, et al. Positive rates and factors associated with abnormal lung function of greenhouse workers in China: a cross-sectional study. International Journal of Environmental Research and Public Health. 2017; 14 (9): 956.
12. Doust E, Ayres JG, Devereux G, Dick F, Crawford JO, Cowie H, et al. Is pesticide exposure a cause of obstructive airways disease?. The European Respiratory Review. 2014; 23 (132): 180–92.
13. Pathak MK, Fareed M, Srivastava AK, Pangtey BS, Bihari V, Kuddus M, et al. Seasonal variations in cholinesterase activity, nerve conduction velocity and lung function among sprayers exposed to mixture of pesticides. Environmental Science and Pollution Research. 2013; 20 (10): 7296–300.
14. Alif SM, Dharmage SC, Benke G, Dennekamp M, Burgess JA, Perret JL, et al. Occupational exposure to pesticides are associated with fixed airflow obstruction in middle-age. Thorax. 2017; 72 (11): 990–7.
15. Lytras T, Kogevinas M, Kromhout H, Carsin A, Antó JM, Bentouhami H, et al. Occupational exposures and 20-year incidence of COPD: the European community respiratory health survey. Thorax. 2018; 73 (11): 1008–15.
16. Mohammadien H a., Hussein MT, El-Sokkary RT. Effects of exposure to flour dust on respiratory symptoms and pulmonary function of mill workers. Egyptian Journal of Chest Disease and Tuberculosis. 2013; 62 (4): 745–53.
17. Mamane A, Baldi I, Tessier JF, Raherison C, Bouvier G. Occupational exposure to pesticides and respiratory health. European Respiratory Review. 2015; 24 (136): 306–19.
Recommended Citation
Nurcandra F , Mahkota R , Miko Wahyono TY ,
et al.
Adverse Effect of Aerosol Pesticide on Lung Dysfunction amongPaddy Farmers in Purworejo, Central Java, Indonesia.
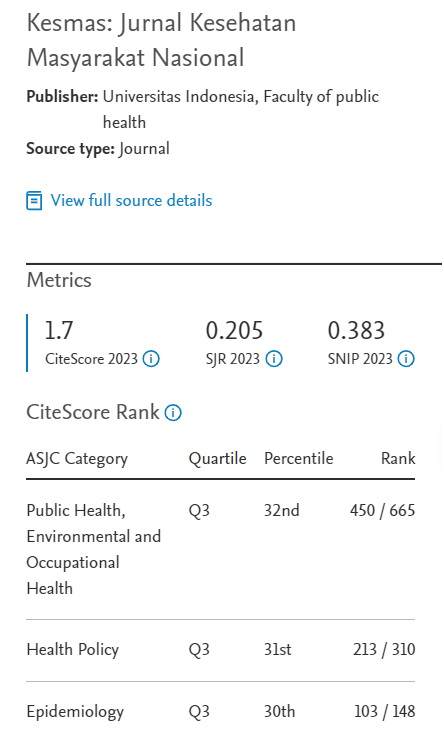
Kesmas.
2020;
15(2):
92-98
DOI: 10.21109/kesmas.v15i2.2703
Available at:
https://scholarhub.ui.ac.id/kesmas/vol15/iss2/7
Included in
Biostatistics Commons, Environmental Public Health Commons, Epidemiology Commons, Health Policy Commons, Health Services Research Commons, Nutrition Commons, Occupational Health and Industrial Hygiene Commons, Public Health Education and Promotion Commons, Women's Health Commons