Abstract
Zika virus can be transmitted through mosquitoes such as Aedes aegypti and Ae. albopictus. During the transition period of 2014–2015, an outbreak of dengue was reported in Jambi City, during which several sufferers were screened positive for Zika virus infection by the Eijkman Institute. It was interesting to note that all of those positive for Zika virus infection were indigenous residents and none of them had a history of international travel. This descriptive analytic study with a cross-sectional design study was conducted to present an overview of Aedes spp. population using ovitrap and egg colonization methods and to detect the presence of Zika virus. Samples were analyzed using reverse transcription polymerase chain reaction for detection of Zika “like” virus and the mapping results were described. The Ovitrap Index was 44.74%, and examination of egg colonization collected from 40 neighborhoods revealed the presence of Zika “like” virus in samples obtained from the fourth neighborhood in Talang Bakung village. This result indicates the occurrence of natural vertical transmission of Zika “like” virus in A. aegypti mosquito in Jambi City, which potentially resulted in an outbreak.
References
1. Zanluca C, Melo VC, Mosimann AL, Santos GI, Santos CN, Luz K. First report of autochthonous transmission of Zika virus in Rio De Janeiro Brazil. Memórias do Instituto Oswaldo Cruz [Internet]. 2015[cited 2018 Mar 8]; 110 (4): 569–572. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4501423/pdf/0074- 0276-mioc-110-4-0569.pdf
2. Kuno G, Chang G-JJ. Full-length sequencing and genomic characterization of Bagaza, Kedougou, and Zika Viruses. Archives of Virologyl [Internet]. 2007 [cited 2018 Mar 8]; 152:687–696. Available from: https://link.springer.com/content/pdf/10.1007%2Fs00705-006-0903- z.pdf
3. Campos GS, Bandeira AC, Sardi SI. Zika virus outbreak Bahia Brazil. Emerging Infectious Disease. 2015; 21(10):1885–1986.
4. Lanciotti, Robert S. Kosoy, Olga L. Laven JJ, Velez, Jason O. Lambert, Amy J. Johnson, Alison J. Stanfield, Stephanie M. Duffy MR. Genetic and Serologic Properties of Zika Virus Associated with an Epidemic, Yap State, Micronesia, 2008. Emerging Infectious Disease. 2008; 14(8):1232–1239.
5. Mark R. Duffy., Tai-Ho Chen MD, W. Thane Hancock, Ann M. Powers, Jacob L. Kool, Ph.D., Robert S. Lanciotti, Moses Pretrick BS, Maria Marfel, B.S., Stacey Holzbauer, Christine Dubray, Laurent Guillaumot, M.S., Anne Griggs, Martin Bel, Amy J. Lambert, Janeen Laven, Olga Kosoy. Zika Virus Outbreak on Yap Island, Federated States of Micronesia. New England Journal Medicine [Internet]. 2009 [cited 2018 Mar 8]; 360(24): 2536–2543. Available from: http://www.nejm.org/doi/pdf/10.1056/NEJMoa0805715
6. Aditya Perkasa, Frilasita Yudhaputri, Sotianingsih Haryanto, Rahma F. Hayati, Chairin Nisa Ma’roef, Ungke Antonjaya, Benediktus Yohan, Khin Saw Aye Myint, Jeremy P. Ledermann, Ronald Rosenberg, Ann M. Powers RTS. Isolation of Zika Virus from Febrile Patient, Indonesia. Emerging Infection Disease [Internet]. 2016 [cited 2018 Mar 8]; 22(5): 924–925. Available from: https://wwwnc.cdc.gov/eid/article/22/5/pdfs/15-1915.pdf
7. Bearcroft WGC. Zika Virus Infection Experimentally Induced In a Human Volunteer. Trans of The Royal Society of Tropical Medicine and Hygiene [Internet]. 1956 [cited 2018 Mar 8];50 (5): 442–448. Available from: http://www.icmr.nic.in/zika/publications/Zika virus experimentally induced.pdf
8. WHO. WHO | Zika situation report [Internet]. WHO. World Health Organization; 2016 [cited 2018 Mar 8]. Available from: http://www.who.int/emergencies/zika-virus/situation-report/28-july2016/en/
9. Javois L. Immunocytochemical methods and protocols. [Internet]. Second. New Jersey: Humana Press; 1999 [cited 2018 Jun 3]. Available from: https://www.google.com/
10. Kendall, L.V., and Riley L. Reverse transcriptase polymerase chain reaction (RT-PCR). The American Association Laboratory Animal Science [Internet]. 2000 [cited 2018 Jun 1];39 (1):42. Available from: https://www.ingentaconnect.com/content/aalas/jaalas/2000/00000039 /00000001/art00008?crawler=true
11. Lee HL. Aedes ovitrap and larval survey in several suburban communities in Selangor, Malaysia. Tropical Biomedicine [Internet]. 1992 Dec 5 [cited 2018 May 30]; 9(1):9–15. Available from: https://eurekamag.com/research/002/293/002293906.php
12. Fatmawati Titi, Ngabekti Sri PB. Distribusi dan kelimpahan populasi Aedes spp. Di Kelurahan Sukorejo Gunungpati Semarang berdasarkan Peletakkan Ovitrap. Unnes Journal Life Science [Internet]. 2014 [cited 2018 Jul 8]; 3(2): 130–139. Available from: http://studylibid.com/doc/972071/unnes-journal-of-life-science
13. Satoto TBT, Alvira N, Wibawa T, Diptyanusa A. Improvement to early warning system the transmission of Dengue fever through controlling potential factor in Public Elementary School At Yogyakarta. Kesmas National Public Health Journal. 2017; 11(4): 178-184
14. Lanciotti, R S Calisher, C H Gubler, D J Chang, G J Vorndam A V. Rapid detection and typing of Dengue viruses from clinical samples by using reverse transcriptase-polymerase chain reaction. Jornal of Clinical Microbiology [Internet]. 1992 Mar [cited 2018 May 28]; 30(3): 545– 551. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1372617
15. Balm, Michelle N.D. Lee, Chun Kiat Lee, Hong Kai Chiu, Lily Koay, Evelyn S.C. Tang JW. A. Diagnostic polymerase chain reaction assay for Zika virus. Journal of Medicine Virology Internet]. 2012 Sep [cited 2018 May 30]; 84(9):1501–1505. Available from: http://doi.wiley.com/10.1002/jmv.23241
16. Tesh RB, Guzman H, Hart CE, Huang J, Thangamani S. Vertical Transmission of Zika virus in Aedes aegypti mosquitoes. American Jounal of Tropical Meicine and Hygiene [Internet]. 2016 November 2 [cited 2018 Jun 3]; 95(5):1169–1173. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27573623
17. Honório NA, Silva W da C, Leite PJ, Gonçalves JM, Lounibos LP, Lourenço-de-Oliveira R. Dispersal of Aedes aegypti and Aedes albopictus (Diptera: Culicidae) in an urban endemic Dengue area in the State of Rio de Janeiro, Brazil. Memorias do Insituto Oswaldo Cruz [Internet]. 2003 Mar [cited 2018 Aug 9]; 98(2):191–198. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0074- 02762003000200005&lng=en&tlng=en
18. Clark GG, Anderson RA, Amador MA, Reiter P. Short report: dispersal of Aedes aegypti in an urban area after blood feeding as demonstrated by rubidium-marked eggs. American Journal of Tropical Medicine and Hygiene [Internet]. 1995 Feb 1 [cited 2018 Aug 9];52(2):177–179. Available from: http://www.ajtmh.org/content/journals/10.4269/ajtmh.1995.52.177
19. Schatzmayr HG. Dengue situation in Brazil by year 2000. Memorias do Insituto Oswaldo Cruz [Internet]. 2000 [cited 2018 Aug 9];95(suppl 1):179–181. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0074- 02762000000700030&lng=en&tlng=en
20. Cahyati WH, Sukendra DM, PS YD. Penurunan container index (CI) melalui penerapan ovitrap di Sekolah Dasar Kota Semarang. Unnes J Public Health [Internet]. 2016 Oct 28 [cited 2018 Jul 17]; 5(4): 330. Available from: https://journal.unnes.ac.id/sju/index.php/ujph/article/view/13965
21. Marchette NJ, Garcia R, Rudnick A. Isolation of Zika virus from Aedes aegypti mosquitoes in Malaysia. American Journal of Tropical Medicine and Hygiene [Internet]. 1969 May [cited 2018 Jun 1];18(3):411–415. Available from: http://www.ncbi.nlm.nih.gov/pubmed/4976739
22. Boorman JP, Porterfield JS. A Simple technique for infection of mosquitoes with viruses; transmission of Zika virus. Transactions of The Royal Society of Tropical Medicine and Hygiene [Internet]. 1956 May [cited 2018 Jun 1]; 50(3):238–242. Available from: http://www.ncbi.nlm.nih.gov/pubmed/13337908
23. Cornet, M., Robin, Y., Adam, C., Valade, M., Calvo MA 1979. comparison between experimental transmission of yellow fever and Zika Viruses in Aedes aegypti [arbovirus diseases, Ethiopian region, Senegal]. Cah ORSTOM Serie Entomol Medicale Parasitol [Internet]. 1979 [cited 2018 Jun 1];17: 47–53. Available from: http://agris.fao.org/agris-search/search.do?recordID=XE8036808
24. Wong P-SJ, Li MI, Chong C-S, Ng L-C, Tan C-H. Aedes (Stegomyia) albopictus (Skuse): a potential vector of Zika virus in Singapore. Turell MJ, editor. PLoS Negleted Tropical Diseases [Internet]. 2013 Aug 1 [cited 2018 Jun 1]; 7(8):e2348. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23936579
25. Zanluca C, Melo VCA de, Mosimann ALP, Santos GIV dos, Santos CND dos, Luz K. First report of autochthonous transmission of Zika virus in Brazil. Memorias do Insituto Oswaldo Cruz [Internet]. 2015 Jun 9 [cited 2018 Mar 8]; 110(4):569–572. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0074- 02762015000400569&lng=en&tlng=en
26. Sasmono, T., Yohan, B., Setianingsih, T.Y., Aryati, Wardhani, P., Rantam FA. Identifikasi genotipe dan karakterisasi genome virus Dengue di Indonesia untuk penentuan prototipe virus. In: Prosiding InSiNas 2012. 2012. p. (422) 1-6.
27. Andriyani Y. Deteksi dan penentuan serotipe virus Dengue tipe-3 (Den3) dari nyamuk Aedes Aegypti dengan menggunakan reverse transcriptase- PCR (RT-PCR) di Kota Medan [Internet]. USU, Medan; 2009 [cited 2018 Jun 1]. Available from: http://repository.usu.ac.id/handle/123456789/6230
Recommended Citation
Satoto TB , Pasca Wati NA , Purwaningsih W ,
et al.
Occurrence of Natural Vertical Transmission of “Zika like Virus” in Aedes aegypti Mosquito in Jambi City.
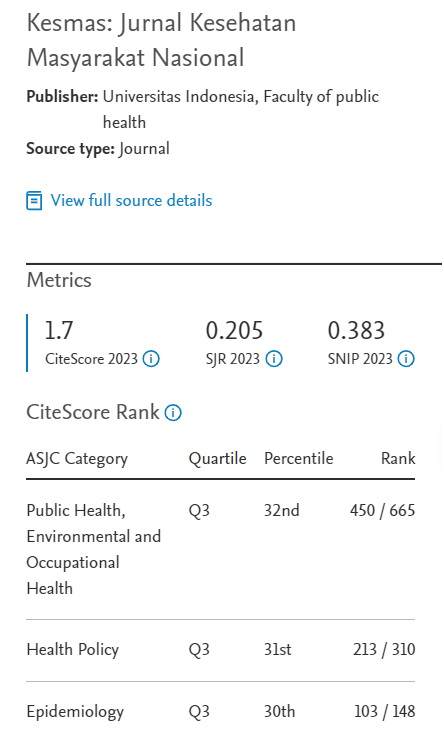
Kesmas.
2019;
13(4):
189-194
DOI: 10.21109/kesmas.v13i4.2709
Available at:
https://scholarhub.ui.ac.id/kesmas/vol13/iss4/6
Included in
Biostatistics Commons, Environmental Public Health Commons, Epidemiology Commons, Health Policy Commons, Health Services Research Commons, Nutrition Commons, Occupational Health and Industrial Hygiene Commons, Public Health Education and Promotion Commons, Women's Health Commons